Less than one percent of the world’s population has it. I’m talking about Infantile VEO-IBD, or “Very Early Onset” IBD. What’s that you may wonder? It’s a rare and often fatal subset of Crohn’s disease that impacts children ages two and under. This week we hear from a mom whose daughter Riley was diagnosed with Infantile VEO-IBD as a newborn, she’s now 18 months. During her first year of life, Riley spent 27 weeks in the hospital. Jana Gilkey opens up candidly about what it’s like to be this type of IBD mom, what she wants others to know about her daughter’s patient journey, and how you can best support families with medically complex children.

Clinical characteristics of Infantile IBD are different from those of an adolescent or adult-onset case with features that are more aggressive & rapidly progressive. There is no known treatment plan and no known cure. Much of the treatment and therapies available are considered research and trial based and are not currently approved by the FDA due to the young age of those diagnosed.
Jana says she could tell something was off from the moment Riley was born. At first as an exclusively pumping mama, she thought her daughter had a dairy intolerance, so she cut every common allergen from her diet.
“We saw our first pediatric gastroenterologist when Riley was one month old. As a mom, my intuition was screaming at me that something was terribly wrong. We saw a few different pediatric gastroenterologists and by month two of life, her symptoms had only progressed. By the time she was 3 months old, she was not stable enough to stay home and had completely stopped eating by mouth. What little we could get her to eat, she was unable to keep down. She was diagnosed with failure to thrive and rapidly declining on all accounts.”
Riley was hospitalized for the next three months. Every day brought new symptoms and complications. She had been evaluated for every condition and received her first PICC Line in which she received continuous TPN & Lipids due to not tolerating any kind of substance in her stomach. Riley also received a series of blood, iron, and albumin transfusions.

Receiving the Infantile VEO-IBD diagnosis
An upper and lower endoscopy revealed lesions throughout Riley’s entire GI Tract. Bingo.
“I began to scour the internet on anything and everything I could find on Infantile VEO-IBD. There was a white board in our hospital room. I wrote down everything I could find on that board. I drew myself diagrams and made notes on doctors to try and connect with. I recorded nearly every second of my daughter’s day those 3 months of our first hospital stay. I ordered books and searched and listened to every podcast I could find on children diagnosed with autoimmune diseases in the first few months of life. I fell asleep most nights watching YouTube videos on nearly every kind topic you can imagine regarding genetics, the immune system, how the body processes monosaccharides, how the brain communicates to the GI tract, and everything else in between I could find to better understand, educate, and advocate for my daughter.”

Like anyone with IBD can relate to—the unpredictability and uniqueness of each person’s experience with IBD makes a diagnosis extremely challenging to cope with.
“While all of my research and studies have been vital to my education and understanding, the very best education (and support) we have received has been from those who also walked a similar journey battling Infantile VEO-IBD.”
How it feels to watch your baby fight a chronic illness
The way Jana describes what it’s like to be a mom watching your child fight an uphill battle against their health had me crying. She explains her experience and perspective so beautifully, yet it’s heart-wrenching to read.
“Most of the time it feels like frantically trying to catch little fireflies that show a glimmer of themselves and then seem to disappear just before jarring them all up. Impossible to fix and yet, aren’t good moms supposed to fix things for their babies? It feels like trying to catch water in the cup of your hands. It just keeps slipping through, no matter how tightly you squeeze. To me, watching my daughter endure such chronic pain and struggle, feels like a constant dance between surrender and war.”
You can feel the pain and the love in her words.
“When Riley was first diagnosed. I was ready to fight, on a mission to find a cure, fly her anywhere, climb the highest mountain, swim to the bottom of the ocean to find that one special pearl that could bring her healing. I believed (and still believe) that the healing remedy for her is out there. However, I have since come to terms that the journey we are on is not a sprint. It is a marathon. I surrender to the things which I cannot control or change. But I will never stop fighting for better. I am willing to run this marathon for the rest of my life so that, Lord willing, my daughter or maybe even those that come after her don’t have to.”

How IBD has “given” to Jana’s family more than it’s taken
Jana says Riley’s disease has changed everything about her outlook on health and her overall perspective on life in general.
“I believe it has given to our family more than it has taken. Riley’s battle with Crohn’s Disease may have robbed us of nearly all of her first year of life on what “could have been.’’ However, it has given us as a family the opportunity to choose what is and what can be. We have been given the opportunity to choose joy during uncertainty and at times chaos.”
Through the pain and tears Jana has realized that we do not own our health but steward it.

She says, “health is not ours to claim but to honor and look after. While it may at times feel as if I have somehow failed my daughter’s health, this is not true. I have honored it with all it has brought. It was never within my control to begin with. I believe the same is true for others within the chronic illness world. There is a lot of room for grace here.”
A life-threatening setback
Riley recently was unable to absorb any nutrients in her GI tract. She started refusing to take anything by mouth and was provided nutrients intravenously through a catheter in her chest the first 10 months after her initial Infantile VEO-IBD diagnosis. The hope—once the right combination of medications was found to wrangle Riley’s disease under control that a gastrostomy tube (g-tube) could be placed.
“One of the many risks of living life with a central line can be infection of the blood. Riley was at high risk for infections due to the medications she was receiving for treatment in addition to being immunocompromised. Unfortunately, Riley developed a blood infection on three different occasions and one put her body in a state of shock.”
Jana says thanks to the grace of God, Riley recovered and does not have any known organ damage at this time. The last four months she’s been home and started to tolerate food in her GI tract. She’s completely weaned from being fed through her veins!

“While we are still searching and longing to find remission for her, she is able to finally have a little more freedom to be the toddler she is. We still have some hard days, but we do feel hopeful we are on the path to remission and will soon see her body heal. Each day that she feels better, we see more of her personality. It is so fun to finally get to know her and see her able to explore more of her world!”
Treating and managing Infantile VEO-IBD
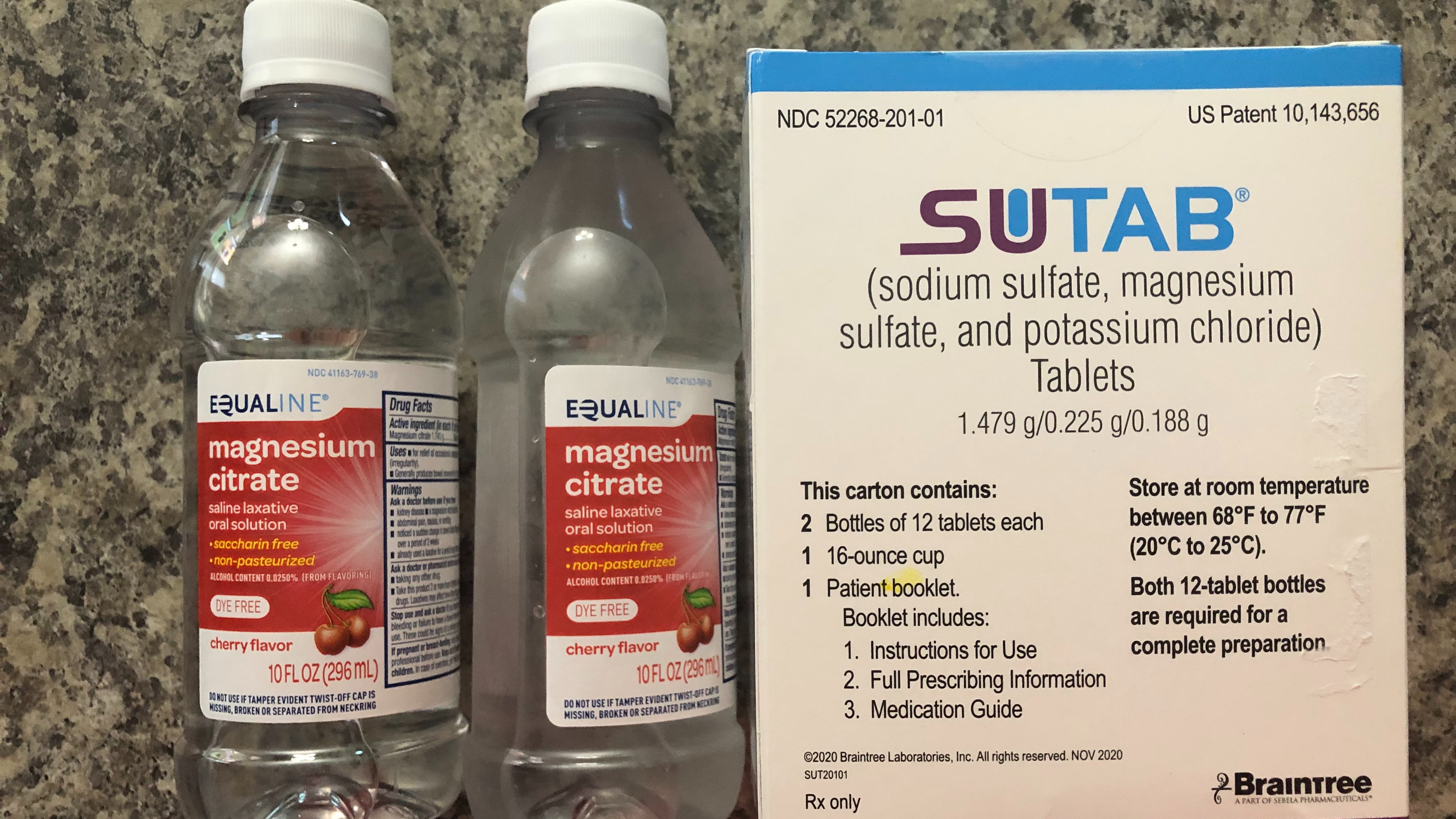
In her 18 months of life, Riley has been on a laundry list of medications and treatments and endured countless procedures and surgeries.
Medications/Treatments
Proton Pump Inhibitors
Liquid, Topical, & Inhaled Corticosteroids
Biologics
Chemotherapy Trails
Glycopeptide Antibiotics
Additional Daily Dietary Supplements
TPN & Lipids
Surgeries:
Multiple Invasive & Non-Invasive Diagnostic Tests and Scopes
Gastronomy Tube Placement
Catheter Placements & Removals
Riley becomes a big sis
This past August Riley became a big sister to Josephine. Since Riley’s health has not been stable enough to travel or be around people because of the pandemic, Jana is FINALLY able to travel back home for the holidays with her family of four. Many of their loved ones met both daughters for the first time this past week at Thanksgiving. Jana says while the lows of Crohn’s disease have been really low, it makes the highs feel that much higher. As she juggles life with a medically challenged child and a healthy child alongside her husband, she’s trying her best to enjoy being a “mom” instead of solely a caretaker.

“While it is very busy, I will say, that in a way my second born has helped us all to take a breather as a family. It’s helped to remind me that I am their mother still and more than a caretaker to both of them. Up until recently, our life has been about keeping Riley here with us. Thankfully, she is in a much better place, and I can also focus on raising her and her baby sister together! This would all be so much more tough without our wonderful support system we have. My husband is unbelievably helpful in addition to my own mother who has been with us every step of the way in this journey.”
Jana says having tangible support is a huge stress relief. By tangible she means, physical help with chores around the house like doing dishes, the laundry, and even having family members learn how to manage a g-tube so her and her husband can take a nap every now and then.

“None of it is how I envisioned our life going and it sure isn’t perfect, but I would not trade either of my girls for one second. I believe every child comes to the world at the time they are destined to come. I know they are meant to be here at the time they are and together.”
How IBD has impacted motherhood from a parent perspective
Jana says she no longer looks forward to the expectations she may have had for her children. Instead, she looks forward to watching whatever they choose to paint the canvas in front of them.
“It’s actually so much more exciting to not have expectations, just enjoying what I can from each day with them, and on the edge of my seat to cheer them on in whatever they do. They are God’s children, and it is a great honor and challenge for me to be able to steward them well. I trust He will fight for them and will always be with them even when I can’t.”
The journey over the past 18 months has helped Jana gain a better understanding of fellow moms as well.
“What may be best for one family may not be best for the next and that is something to celebrate really – not be judgmental or weary of. Moms have way too much on their backs to place any judgement. The children we have been given were given to each of us as individuals for a reason and no one else. There is no longer room for guilt or judgement here, just grace and support.”
Best ways to support families with medically complex children
When loved ones and friends go through health hardships, we often want to help in some way. But unbeknownst to us some of the ways we approach the conversations can be off-putting without even realizing it. Jana says knowing so many people (many whom they have never met) are praying for Riley, interested in her journey, and supporting them, has been incredibly overwhelming.
“I met so many truly inspiring families and individuals over the last year and a half since Riley’s diagnosis. Sometimes, it can be exhausting to share our story, as there is so much to explain. But, each time I share, I am reminded that we are not alone in this. That is really a huge encouragement when times have felt isolating.”

Jana has come to realize that when it comes to health and those walking through a medical journey, that what we may know or what they choose to share about their story is often just the tip of the iceberg to what they are going through.
“Offer grace, not judgement. Offer time, not advice. People genuinely mean it when they say, “Let me know how I can help.” These questions are well meaning but they put the ball in the court of the person who may be enduring rather than the one seeking to support. It’s often difficult to understand what your own needs may be when in seasons of crisis.”
Instead seek to understand. While it feels natural to ask questions like, “Are you/they feeling better?, “How was your day?”, or “What can I do to help?” These types of questions can feel broad and difficult to answer in the world of chronic illness.
Jana recommends asking questions to seek understanding. She says asking the right questions can be helpful for those we want to support.
Here are some examples:
- Can you tell me about your day today?
- I spent some time researching the diagnosis you shared with me, and I have a few questions…would you mind if I asked you so I can better understand what it looks like for you?
- I would like to know more about what the days look like for you. Would you like to share?
- How does your daughter’s diagnosis and patient journey affect you?
Want to do something spontaneous, without asking? Go for it. Deliver a meal, write a letter, offer your time in a way that does not require a friend who may be in crisis to ask things of you. Pain can often feel like a burden and be very isolating. Having someone ask to better understand and invite themselves into our pain helps to lift that burden – just knowing someone else sees.