Crohn’s disease and ulcerative colitis can cause symptoms both in and out of the gut. When our disease wreaks havoc on other parts of our body, outside of our intestines, it’s known as an extraintestinal manifestation (EIM) or complication. Did you know, according to the Crohn’s and Colitis Foundation, anywhere between 25-40% of people with IBD experience some type of EIM? EIMs arise in the joints, skin, eyes, bones, kidneys, and liver or as anemia. This week on Lights, Camera, Crohn’s a deep dive into the heavy toll of living with not only IBD but the EIMs that come along with them and how more than 30 patients manage these issues that can significantly impact the quality of life and overall health of IBD patients.

One of the most interesting quotes from a patient was that while one man doesn’t like EIMs, he’s grateful for them because that’s often the only time family, friends, and medical providers can see with their own eyes what a serious illness IBD is. It’s heavy, but it makes sense. IBD is so much more than a bathroom disease and EIMs go to show how severe Crohn’s and ulcerative colitis can be and how this is a full body disease.
The most common EIMs associated with IBD
- Joint problems: This is the most common EIM and affects around 25% of IBD patients. The pain normally occurs in the knees, ankles, and wrists, but can also happen in the spine in the form of ankylosing spondylitis. For many of us, our biologics or biosimilars are approved to treat both IBD and rheumatoid arthritis and this can help alleviate joint pain.
- Skin Conditions: The two main conditions are Erythema nodosum and Pyoderma gangrenosum. EN is characterized by tender red nodules that usually occur on the shins. PG is a more severe skin condition that causes painful ulcers. Those with IBD also have a greater chance of developing skin tags, anal fissures, and fistulas, both Enterocutaneous (from the intestine to the skin) and Perianal (around the anus that can drain blood, pus, and/or stool.
- Eye Disorders: When those with IBD deal with red eyes, pain, and vision problems, uveitis and episcleritis tend to be the culprit.
- Kidney complications: Medications tend to cause this, and serious kidney complications associated with IBD are rare, but still can happen in the way of kidney stones, hydronephrosis (an obstruction of the ureters, which connect the kidney to the bladder), and fistulas (abnormal connections between the intestines, bladder, or ureter). Amyloidosis (an abnormal deposit of protein in the kidneys) and Glomerulonephritis (inflammation in the kidney that limits its ability to filter properly) can also occur.
- Liver and Biliary Tract Diseases: Primary sclerosing cholangitis (PSC) is a serious liver disease is most commonly seen in conjunction with ulcerative colitis. This is often discovered when lab works show liver markers are out of whack and it’s diagnosed with a liver biopsy to determine the stage and level of severity. Fatty Liver Disease, Hepatitis, and Gallstones are also considered EIMs.
- Bone Health Issues: Osteoporosis and osteopenia can result from years of chronic inflammation, steroid use, and malnutrition. It’s a good idea to get a baseline DEXA bone scan and to get scans periodically to make sure you’re not experiencing this.
- Lung Issues: While this is less common, lung involvement can include airway inflammation and interstitial lung disease.
Managing EIMs along with your IBD
Managing and treating EIMs is no easy feat and often necessitates a multidisciplinary approach, including your gastroenterologist, rheumatologist, dermatologist, and other specialists, depending on what organs are affected. Treatment strategies might include non-steroidal anti-inflammatory drugs (NSAIDs), immunosuppressive medications, and biological therapies which are tailored to reduce inflammation and manage symptoms.

You may wonder if there’s any way to prevent EIMs from happening in the first place. There are several strategies that can help reduce your risk, but much like anything with IBD, don’t blame yourself if EIMs keep happening to you and feel out of your control.
- Effective IBD Management: Controlling your IBD through appropriate medical therapy is crucial, whether that’s in the way of aminosalicylates, steroids, immunomodulators, and biologics/biosimilars. The goal is to reach and sustain remission of your IBD, which can help reduce the risk of EIMs popping up.
- Communicating when you see a change: Once you notice a possible EIM, it’s imperative you share this with your healthcare provider. Early detection and treatment of EIMs can prevent them from getting more severe. A simple message on the Portal to your GI addressing your concern or worry helps alert your doctor so they can take the appropriate measures before symptoms spiral out of control.
- Lifestyle Modifications: Smoking is known to worsen the course of IBD and increase the risk of EIMs, especially in Crohn’s disease. Consulting with a dietitian who specializes in IBD can help ensure you are receiving adequate nutrition and getting regular exercise can help reduce inflammation, improve bone health, and enhance your overall wellbeing. Speaking of bone health, calcium and vitamin D supplements can help counteract the lasting effects of steroid use and malnutrition.
- Collaborative Care: By branching out from your GI and seeking care from specialists, you have the best bet of ensuring EIMs are treated promptly and effectively. Talk with your GI about the potential signs and symptoms of EIMs so you know what to watch out for and have a game plan in place if one were to arise to feel more in control.
Medical gaslighting and EIMs
Unfortunately, far too many patients and caregivers feel symptoms are dismissed or not taken seriously by healthcare providers, which can be particularly discouraging and frustrating.

“I had a tough time getting my consultant to take me seriously. The eye problems were “probably just bad eye strain,” the mouth ulcers were “maybe the cups in the office not properly being cleaned, and the rashes were “probably a reaction to laundry detergent or maybe insects getting on my clothes while they are on the clothesline outside.”
Here are some helpful strategies to help you speak up in these situations and feel empowered to advocate for your health effectively:
- Document Your Symptoms: You may think you’ll remember what’s going on, but life with chronic illness gets hazy and when we think back, we can lose sight of the actual frequency and intensity of what we’re going through. A detailed diary will help provide concrete evidence to discuss with your healthcare provider and may even help assist in identifying patterns that are relevant to your diagnosis and treatment.
- Seek Second Opinions: If you don’t feel listened to or heard, don’t hesitate to get a second opinion, and find a provider you jive well with. Each doctor has varying levels of experience with IBD and EIMs, find the person who best understands your personal situation and is willing to get you to where you need to be, rather than dumbing down or belittling your experience.
- Be Prepared for All Appointments: Write down a list of questions and concerns before your appointments. Bring your symptom diary and any other relevant medical records. By being prepared, you can better focus and ensure that you’re capitalizing on the one-on-one time you have with your doctor while you’re face to face.
- Bring an Advocate: Having a trusted friend or family member at your appointment can provide support and help ensure that your voice is heard. That person can also help remember details on the appointment that you may not.
- Be Clear and Assertive: There is a delicate balance between being assertive about your concerns without being confrontational. Be descriptive and transparent about the impact your symptoms have on your daily life, paint as clear a picture as you can and explain why it’s important for these symptoms to be addressed.
- Educate Yourself: By understanding what EIMs are ahead of your appointment you can feel more confident about asserting your concerns and how best to improve your health. If you’re able to “talk the talk” with medical language about your condition, your healthcare professional will be more apt to listen.
- Formal Complaints: If you repeatedly feel as though you’re dealing with an unprofessional doctor who has a dismissive attitude, or if you feel your care is compromised, it may be necessary to share a formal complaint with the medical facility.
Let’s hear from IBD patients and caregivers
Leah daughter was diagnosed with Crohn’s when she was five.
“Little did we know our most difficult days would come a few years later and be due to an extraintestinal manifestation of her IBD. It started off as bruises on my daughter’s shins. I thought it was related to her sledding on her knees with the recent snowfall. Unfortunately, I had never learned about Erythema nodosum being related to IBD and would later learn this is what she had. The spots on her legs grew and grew. They eventually got raised and painful. I emailed our GI nurse and thankfully she instantly knew and sent us for stat labs. My daughter was on Humira and wasn’t in remission, so the drug was increased. Week by week things got worse and more painful. The redness and swelling covered her entire shins. The bumps spread to the bottom of her feet and were extremely painful. Her feet swelled and she was crying in pain and no longer able to walk on them.”



Leah ended up taking her daughter to the ER where she got steroids and started on antibiotics as it looked like the spots had turned into cellulitis on her feet.
“I was not prepared that EN could be associated with IBD. I wish I had known earlier, so her condition could have been treated more aggressively from the beginning. It was many months before she healed, and her maintenance medication was switched.”
Emilie– “This is such an important topic and I wish it were discussed more! Most of my UC complications have revolved around extraintestinal manifestations (as opposed to typical UC symptoms). I have had arthritis and uveitis and for me, extraintestinal manifestations always come first, before a typical flare and always stay long after the typical UC symptoms have resolved. At times, I’ve just had extraintestinal manifestations without any typical UC flare symptoms. The most frustrating part about EIM symptoms is that most GI doctors aren’t super familiar with them and only think they happen after a UC flare. Thankfully, I’ve been followed by a rheumatologist since I was diagnosed (because I had EM symptoms long before I had typical UC symptoms and saw a rheumatologist first). My rheumatologist is always like, “we follow people with these symptoms to see if they develop IBD” and many of my GI doctors have said, “this can’t be because of your UC.”
Dina was diagnosed with UC in January 2022 after experiencing IBD-related symptoms six months prior. Since then, she’s had pneumonia, mono, CMV, RSV, and other illnesses. She went from weighing 150 pounds to 120 and was so weak she could barely walk. She was switched to Entyvio/Rinvoq as a combo therapy along with an anti-viral drug used to treat HIV to try and keep the CMV virus at bay. The CMV made her liver markers skyrocket, and it was discovered she has Stage 1 PSC, in addition to everything else.
“I consider this a blessing because once I went back on the full dose of anti-viral my liver counts normalized. We never would have known about the PSC until it got severe or at a later stage. My GI said he’s never seen PSC in this early stage, so I’m grateful we can start earlier than most to monitor it.
Lynette-“I’ve dealt with many EIMs. To manage my anemia, I take iron and having a hysterectomy helped. For my kidney stones, I stay hydrated with electrolytes daily. I had surgery for hemorrhoids and fistulas. I’m on medication to manage my joint pain and use my heating pad. I use a special toothpaste to prevent cavities and I floss daily. I do everything I can to reduce stress and anxiety—from breathwork, to meditation, and openly communicating with my family.

Madison-“My personal experience is severe joint pain and swelling, as well as erythema nodosum. My IBD flares typically begin with joint pain. At times, it can be so severe I can’t walk up and down stairs because my ankles are so swollen. When I was first diagnosed with Crohn’s, in addition to my joint pain, I started to develop red tender bumps all over my legs up to my knees. They were so painful to touch, and they were diagnosed as Erythema nodosum which only occurs in about 10-15% of Crohn’s patients. Once we got my IBD under control and found the underlying cause of my joint pain and erythema nodosum they thankfully got better.”


Myisha- “I experience inflammation in my eyes three to four times a year. I also deal with osteoarthritis. Mentally, I’ve checked out on my Crohn’s awhile ago. I just take it day by day. I have eye drops that I have to use daily to help with inflammation, but osteoarthritis is painful and some days I want to cut my limbs off. I always try to remind myself that someone out there has it worse and today might be a high pain day, but the darkness doesn’t stay around forever, eventually the sun will shine again, and I’ll have a low pain day.”

Christopher- “I’m 46. I was diagnosed with Crohn’s about two years ago. Three years before that I began having panic attacks and anxiety out of nowhere. I went from never having anxiety or panic to multiple incidents per week. At the same time, I had new joint pain in my knees, and developed arthritis in my shoulder joint as well as mild lower right quadrant pain. Now, looking back, these were all related to systemic inflammation from the undiagnosed Crohn’s. Now that I’m in remission, it’s all gone away.”

Vern– “OMG EIMs!?! I have so many. Along with Crohn’s, I have developed Gilbert’s Syndrome, short gut, Reynaud’s, rigors, kidney stones, skin problems, anemia, B12 and vitamin D deficiency, joint pain, fissures, fistulas, and hair loss. There’s not much to do when it comes to Gilbert’s, Reynaud’s, rigors, or skin…but with kidney stones I drink a lot of water everyday plus cranberry juice or tea every once in awhile. To manage my anemia, B12 and D, I take easily soluble supplements and B12 shots every month. I take Tylenol to manage my joint pain and rest. The fissures and fistulas have a mind of their own, so not much I can do until it’s taken care of surgically if it gets bad enough. The hair loss is from medication and even when I tried different treatments (home remedies) nothing worked until I was off the medication.”
Pao-“I have been experiencing skin issues for the last year and a half. I have a lesion under my armpit, behind my ear, and a gangrenous epidermis, which is healed. I had a biopsy on the lesion and then a corticosteroid cream healed it. The lesion on my ear won’t go away after months of putting cream on it.”
Kerry-“I deal with intense joint and muscle pain all over my body. My left hand got so swollen at one point that I tried to learn to write with my right hand. This was during my initial diagnosis. Once I started on Remicade it helped and now my joint pain is an indicator of disease activity for me. I log symptoms using the Wave app, I increase my rest, and use diclofenac gel as a topical analgesic. I also see a rheumatologist who has experience treating other IBD patients.”
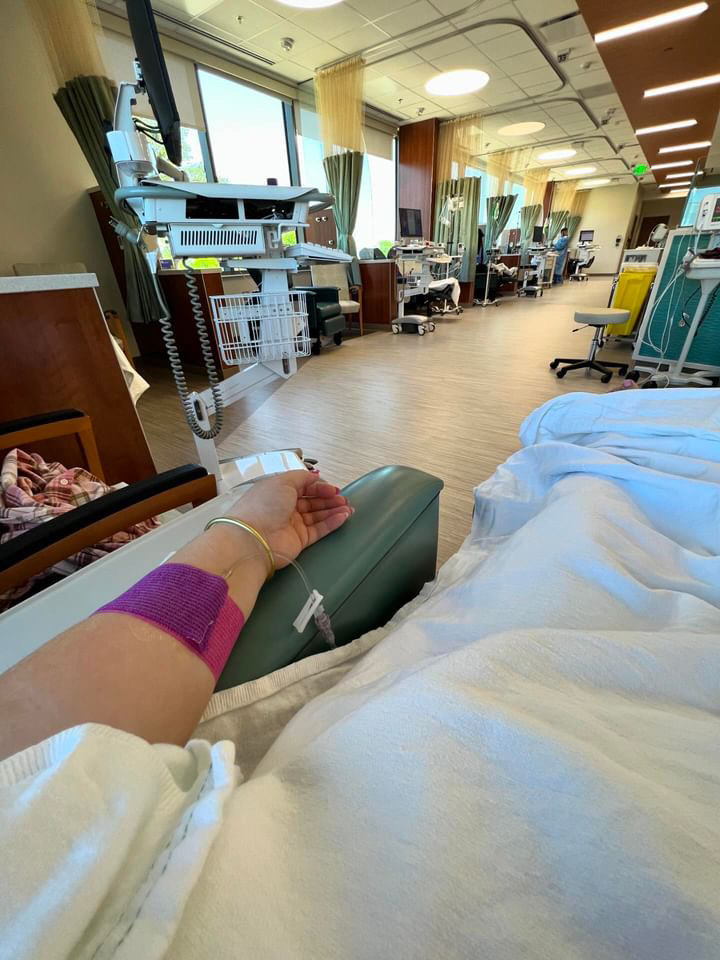
Rocio: “One of my most debilitating and constant EIMs I’ve had over the last 20+ years is iron-deficiency anemia (IDA). The fatigue levels I live with are beyond frustrating. I know the disease itself can add to my fatigue, but even when at my healthiest, I’m constantly tired. And it’s the kind of tired no on understands. I’ve received countless IV iron infusions for my IDA as I can’t tolerate oral iron due to my previous history of chronic constipation. Fortunately, infusions and I’m able to go months without iron, but there have been times where I’ve received 5 infusions in 1 month – yikes!”

One of Rocio’s other debilitating EIMs is uveitis. She says it is truly one of the most excruciatingly painful manifestations.
“Despite having a high pain tolerance due to chronic illness, uveitis has been one experience I don’t wish upon anyone. And uveitis can progress to glaucoma or vision loss. I did have glaucoma along with my uveitis, but we treated it immediately. Due to recurrent uveitis flares and limited treatments that worked for me, I dealt with uveitis for nearly 3 years. The ophthalmological EIMs that can occur with IBD are not one to take lightly…we need our vision!”
The earliest EIM Rocio experienced were perianal fistulas – a common type of enterocutaneous fistulas. Unfortunately, she did not receive proper care initially, or her actual IBD diagnosis, for five years. She could have suffered far less had her fistulas been identified as an EIM of Crohn’s disease.
Jennifer-“So many doctors are just unaware or unwilling to see extraintestinal manifestations for what they are. When I was in my late teens and struggling with depression and a ton of stress in my first year of college, I was shamed by a doctor and told (without any testing) that I had herpes. Mind you, I had never been sexually active and never had symptoms before this point. I was in extreme pain and had painful ulcers from my mouth to my anus and genitalia. I left the appointment in tears and wanted to die. It was only years later that I learned of external manifestations of Crohn’s and had a doctor confirm that is what happening all those years earlier.”
Jennifer says she had far too many unpleasant encounters with doctors over the years. From doctors telling her that she was just a bored homemaker (because he felt my complaints were made up) to dentists shaming her in front of her kids (because her mouth health was in his opinion from lack of hygiene vs. effects of Crohn’s disease).
“I was also told by a GI doctor once that if my Crohn’s disease flared while pregnant that I should just have an abortion (for a pregnancy that I very much wanted). This is not a commentary on my stance on abortion, but rather the lack of empathy and respect that this male doctor had towards me, my health, and my choice in that moment.”
Becky- “Erythema nodosum is so scary and I had no idea what was happening to my legs. It was so painful to even walk. I’ve lived with Crohn’s for 30 years. I was admitted to the hospital and given steroids and the doctors drew black Sharpie circles around the red swollen lumps on my legs to see if they grew larger. I was there several days, and the doctor finally figured out what was going on based off my medical history. I was on steroids for awhile and then it finally cleared up.”

Liz- “Extraintestinal manifestations are one of the toughest parts of Crohn’s for me. I have joint aches, eye inflammation that is so painful and disruptive when it flares and chronic severe anemia. Each result in another doctor, another expensive treatment, and time not feeling well. Getting doctors to recognize that they are all connected is difficult as well.”

Anthony has lived with Crohn’s for almost 18 years and EIMs have been a big part of his journey. To him, they’re often a key indicator that a flare up is on the way and unfortunately EIMs have become a regular part of his life for the past decade.
“I get a lot of eye problems (swelling, overly sensitive to light, foggy vision). Once I woke up with my left eye swollen shut. I get a lot of ulcers on my gums, tongue, and in my throat along with rashes that break out on my arms, back, and hands. When I get ulcers, I have difficulty swallowing and need to consciously put effort into swallowing my tablets and often I’m forced to stay away from solid food and meals.”
Anthony goes on to say EIMs bring on depressive episodes for him, along with brain fog, and having issues concentrating and remembering.
“Some days I wake up at 4 or 5 in the morning with a cement block of sadness in my chest, preparing to go about a “normal” day and hoping not to feel the urge to burst out crying. Before I learned how to live with it and got mental therapy, I had to write almost everything down to the point of keeping a note on my phone with bus and train times that would get me to and from work or to various parts of the city because I’d draw a complete blank at times or couldn’t figure out the timetables. I am an engineer and almost had to give up my career because I couldn’t get through a workday.”
Deb– “I’ve had reoccurring Pyoderma Gangrenosum under the flange or baseplate of my ostomy to the point that the skin and tissue diminished and has now caused a very significantly sized peri stomall hernia. We haven’t landed on a treatment of late that has any amount of effect on the inflammation in my colon, so no hernia repair until we get the CRP way down.”
Courtney-“I’ve experienced blepharitis, which is an inflammation of the eyelid that may commonly be confused with pink eye. I’m not fully clear if it is an extraintestinal manifestation or side effect of immune suppression, but after 5 years “in the clear” it’s back. One of the few occasions when I actually “look sick” but feel fine. It’s treated with antibiotic eye drops. I saw a specialist who recommends a special cleanser with tea tree oil.”
Amanda-“During a particularly bad Crohn’s flare, I developed Erythema nodosum. They were painful welts that went up and down both legs. My legs got so swollen and covered with welts that I couldn’t bend them to walk. It was incredibly painful and difficult to need help just getting out of bed. They took awhile to go down and left bruises all over my legs. No one ever mentioned this to me as a possibility, so I didn’t even think to contact my GI, but my local emergency room doctor pointed me in the right direction.”
Krista– “Oof. Alopecia. I lost probably 50-75% of my hair. Now it’s thicker than it’s ever been. Very strange. I also have experienced bursitis and inflammation in my knees, but that’s only flared up once since my IBD diagnosis.”


Melanie-“I was diagnosed with IBD when I was 12 and by 15, I could no longer walk upstairs due to Crohn’s-related arthritis. I went on Remicade which got me walking again but have since been looking for options. Sometimes my Crohn’s and Arthralgia flare together, but in my experience, when I get one under control, I start having issues with the other one which can make disease management a challenge.”
Tish- “I got Uveitis and must always be on the watch for signs of it now. It was misdiagnosed as an eye infection, and I was sent to the eye and ear emergency, but they also misdiagnosed it. Thankfully, I was able to see my ophthalmologist who correctly identified and treated it properly. I also have very dry eyes, so I always use drops to avoid it leading to another Uveitis flare up.”

Eliza– “I’ve dealt with bone density issues related to my ulcerative colitis. I now take a prescribed high dose of D3 and incorporate calcium and other minerals as often as I can into my diet. I have been getting DEXA scans since I was 19!”
Allison-“Skin!! Why are there no IBD-expert dermatologists anywhere?! Why can’t my doctors give me more information about extraintestinal Crohn’s related skin issues? Are we really suggesting bleach baths as the only path for resolution because that feels insane. I’m struggling to find the right resources to help.”
Stacey-“I developed Type 2 diabetes as a result of the inflammation in my pancreas. In addition to diabetes, I also have Rosacea caused by my Crohn’s. We first thought it was an allergic reaction to my Stelara. However, the Rosacea persisted after I stopped Stelara. I saw a Dermatologist who made the diagnosis, and I was then able to get back on it. Like many IBD patients, I also deal with dry eyes, dry mouth, fatigue, and achy joints.
Dana– “I’ve struggled with cutaneous Crohn’s (perianal and elsewhere) and oral Crohn’s, including mouth sores, gum inflammation, and recession. I’ve been prescribed a lot of various topical medications (tacrolimus, taclonex, steroids…just to name a few). It causes a huge gluteal cleft fissure and a lot of damage to my skin in the perianal area in general, which was resolved when I had my proctocolectomy surgery. They had to cut my rectus abdominis muscle to create a flap and place it in the area where they had to cut out all the tissue and skin. Regarding oral Crohn’s, I have steroid ointment that I use as needed for inflammation/sores and I’ve had three gum graft surgeries so far.”
Gabriella-“I have chronic urticaria and dermatographia that was triggered by a rare reaction to the carrier protein used in Humira and Remicade. The reaction hasn’t gone away despite stopping those medications, and despite taking Xyzal and Benadryl daily. I still have extremely high IgE levels. I had had all the major inflammatory skin conditions associated with Crohn’s as well: Erythema nodosum, Pyoderma gangrenosum, and just general infections from “normal skin flora.” I’ve had multiple bad IBD flares where I’ve experienced inflammatory arthritis in all joints from my hips down.”
Ben-“I was diagnosed with gastroduodenal Crohn’s and UC over 30 years ago when I was six. Back then, it started with Erythema nodosum, which led to a colonoscopy, when then ended in my first polyps removed and a diagnosis. I still have issues with it today. I also picked up an obscure kidney cancer about five years back. My oncology and GI teams feel it is related to my Crohn’s/UC somehow, as they don’t see this type of cancer in patients under age 80. Crohn’s also gives me severe anemia.”
Stephane– “After 15 years of partial obstructions, during which I amazingly enough, managed to avoid diagnosis or treatment, it was the obviousness of an extra-intestinal manifestation, my left ankle swelling for no reason, which marked the beginning of the end of my epic denial. Over the summer, my knees swelled too, and walking became painful and slow. By September, I couldn’t walk at night because of the pain in my joints and had to crawl to the bathroom. Finally appearing in the ER, sent by my GP, ankles, and knees puffy and swollen, anemic, malnourished and down 30 pounds, the doc only needed to glance at my chart and test results to give me a diagnosis of Crohn’s.”
Amanda-“Extraintestinal manifestations I’ve dealt with include mouth ulcers, inflammation of my eyes (so red!), joint pain (specifically knees and hands), TMD (no classic clicking or popping, just mass inflammation of the joint and muscles), eczema, anxiety, slow wound healing, fatty liver (non-alcohol, I don’t drink, I am a fitness and nutrition professional so I know my lifestyle is on point), and kidney stones.
Amanda manages this by having exceptional oral hygiene. She brushes and flosses twice a day and uses Orajel mouth wash. She sees an Ophthalmologist to ensure she doesn’t have damage to her eyes and uses Lumify drops to combat the redness. Amanda takes a curcumin supplement (primary bioactive substance in turmeric) for its anti-inflammatory properties, which may also help with joint pain. She uses a bite splint and warm compresses for her TMD and eczema patches on her face, around her ears, eyes, and neck. Amanda has two different prescriptions from her dermatologist to address this: hydrocortisone cream and fluocinolone oil. She also uses Skin Smart antibacterial eczema spray every night. To deal with the remainder—she practices stress reduction when and where she can, continues to focus on her diet and weightlifting and keeps her sugar intake low. She doesn’t drink alcohol and only takes moderate caffeine each day. She’s also hyper focused on micronutrients, specifically fiber, vitamin D, iron, zinc, folate, and B vitamins for overall health and wound healing. Her Avsola infusion for her IBD also is approved to treat Rheumatoid Arthritis so she feels that helps her joints feel significantly better.
Dealing with the mental health challenges of EIMs
Much like IBD, EIMs take a toll on our mental and emotional wellbeing. By seeking mental health support from a psychologist or counselor trained in chronic illness management, you can receive valuable support. Cognitive behavioral therapy (CBT) is particularly effective for managing depression and anxiety associated with IBD. If this article has done anything, I hope it’s shown you that you are not alone and sadly how common these complications are in our community. By simply going on social media and looking up hashtags for your EIM, you will see so many others who are living your reality and can learn a thing or two and feel understood, seen, and heard. There’s so much power that comes from us joining forces as a shoulder to cry on and an ear to listen, even if we’re thousands of miles apart.

By educating yourself and being proactive about what could happen to your body now or in the future, it can help reduce fear and anxiety that is associated with these unexpected and often unruly symptoms.
Additional Resources
Extraintestinal Manifestations of Inflammatory Bowel Disease – PubMed (nih.gov)
Extraintestinal Complications of IBD | Crohn’s & Colitis Foundation (crohnscolitisfoundation.org)
Extraintestinal Manifestations: IBD Symptoms Outside of the Gut – YouTube