At the inaugural Cedars-Sinai IBD and Women’s Health Conference, experts came together to spotlight the unique challenges women face at the intersection of inflammatory bowel disease (IBD) and women’s health. Co-directed by Dr. Puja Khanna, Clinical Director of the IBD Women’s Health Program, and Dr. Maria Abreu, Executive Director of the IBD Institute, the event featured a two-part format: clinical updates for providers and education for patients and caregivers. Topics ranged from fertility and pregnancy to nutrition and mental health.
One of the featured speakers was Neha D. Shah, MPH, RD, CNSC, CHES, Senior Dietitian at the Colitis and Crohn’s Disease Center at UCSF and founder of Neha Shah Nutrition LLC, a private practice specializing in nutrition care for patients with IBD. Her session focused on nutrition updates and strategies to support gut, muscle, and bone health in women with IBD. This week on Lights, Camera, Crohn’s I spoke with Neha, and she zeroed in on something every woman with IBD should care about: how to use nutrition to protect our gut, muscle, and bone health.

Why Nutrition Matters Beyond the Gut
Whether you live with IBD or care for patients, you know that IBD affects much more than the gut. Fatigue, abdominal pain, and debilitating flares that blindside us can make it feel like our whole body is affected. While we know this, it can be complicated to know how to address these specific challenges.
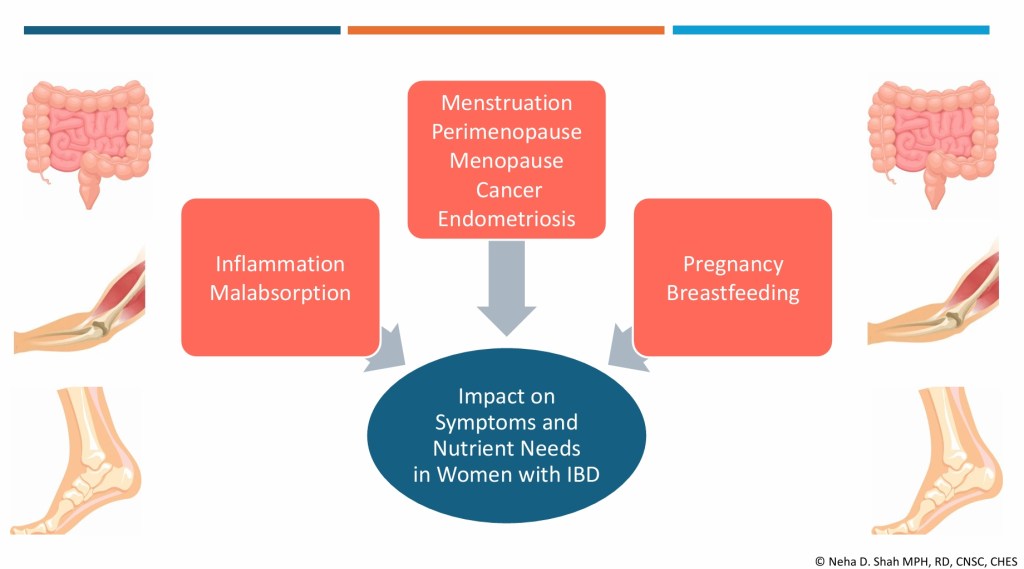
“Women with IBD face a unique set of challenges,” Neha explains. “Poor absorption can contribute to ongoing symptoms, muscle loss, and bone loss. Hormonal shifts, whether from PMS, pregnancy, or perimenopause add yet another layer, often making symptoms unpredictable.”
Her goal? To give women practical, evidence-based strategies they can use to better support their health, both now and as their bodies change through different life stages. As a woman who was diagnosed with Crohn’s disease at age 21, my questions and focus have shifted now that I’m 42 and my family is complete.
“Many women don’t just experience flare-ups; they live with changes in their body that evolve throughout life, impacting daily routines, work, and overall quality of life. In my presentation, I aimed to highlight both the latest updates and practical, whole-food strategies that women can use to better support their health.”
Key Takeaways from Neha’s Presentation
Gut Health
IBD symptoms often overlap with PMS and endometriosis: fatigue, abdominal pain, diarrhea, bloating, and constipation. If you’ve noticed an uptick in your IBD symptoms right around your period, you are not imagining it.
When combined, these conditions can intensify, highlighting the need for careful monitoring and proactive management.
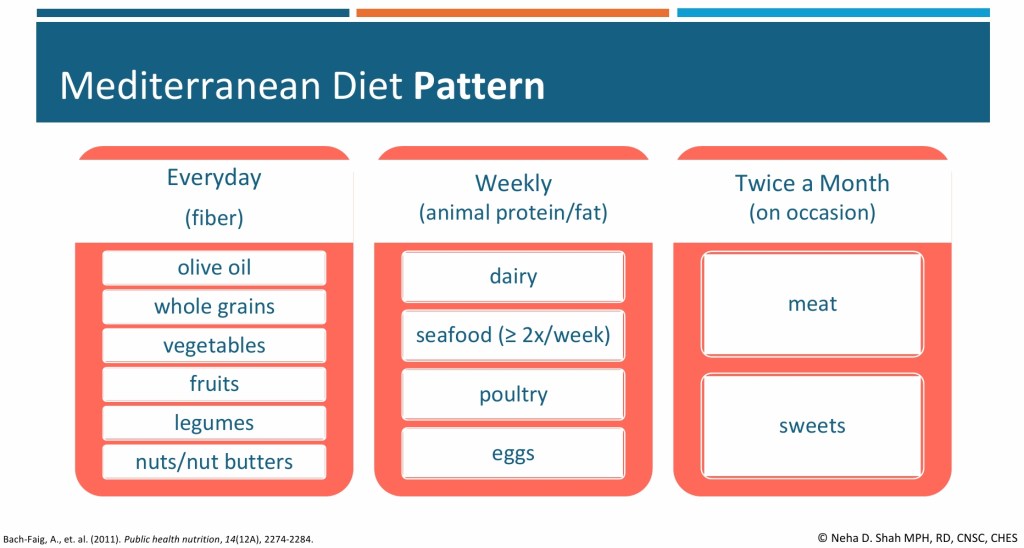
- Dietary Patterns: A Mediterranean-style diet rich in fruits, vegetables, whole grains, legumes, nuts, and olive oil may reduce the risk of IBD flares and ease painful bowel symptoms in women with endometriosis.
- Fiber Matters: Soluble fiber (oats, fruit) can slow diarrhea, insoluble fiber (leafy greens, brown rice) can help constipation, and less fermentable fibers may reduce gas and bloating. Adjusting textures, like blending or mashing can improve tolerance, especially for those with strictures.
Neha notes that further studies are needed here and she’s hopeful we’ll have even more intel in the future.
Muscle Health
Sarcopenia (loss of muscle mass and strength) is more common in IBD due to chronic inflammation and nutrient malabsorption. Hormonal changes and aging further increase the risk.
- Nutrition + Activity: Adequate protein intake (1.2–1.5 g/kg per day for many with IBD) and resistance training are key. Individual requirements sometimes are even higher.
- Gut-Muscle Axis: Emerging research suggests fiber may support muscle health by fueling beneficial gut bacteria. The National Health and Nutrition Examination Survey (NHANES) 2011–2018 survey data from 6,000 healthy adults (without IBD) showed each 5 g increase in fiber intake was associated with higher lean mass and grip strength, possibly through increased short-chain fatty acid production. Fiber’s role in IBD and sarcopenia remains understudied.
- Practical Tip: Aim for 15–20 grams of protein per meal, combining both animal (e.g., fish) and plant-based sources (e.g., lentils, tofu, nut butter). People with IBD generally have higher protein needs, which can vary depending on weight, activity level, and disease state.
“Evidence in women with IBD is limited. One small case-control study of 23 women with UC versus age- and BMI-matched controls found reduced quadriceps strength, slower sit-to-stand and gait speed, and lower physical activity, though handgrip strength was preserved, says Neha. “Early assessment of nutrition, activity, and lower limb function is crucial. No IBD-specific sarcopenia guidelines exist, but recommendations from the International Clinical Practice Guidelines for Sarcopenia by the annual International Conference on Frailty and Sarcopenia Research by centers at John Hopkins University include increasing protein/calorie intake and resistance training.”
Bone Health
Women with IBD are at higher risk for osteoporosis and osteopenia, especially during perimenopause and menopause. The gut-bone axis reflecting the connection between gut microbes and bone health may play a role. Calcium and vitamin D requirements in individuals with IBD depend on factors such as disease activity, malabsorption risk, corticosteroid use, and deficiency status.
If you haven’t done so already, talk with your care team about getting a DXA scan (bone density scan) so you have a baseline. The earlier in your IBD journey, the better. Bone scans are non-invasive, and probably the easiest test we undergo. You wear your street clothes, lie down on a table, and it’s a quick and painless experience. I have a bone health doctor at Wash U (yes, that’s her title!), who focuses specifically on this after a bone scan in 2022 showed signs of osteopenia and osteoporosis in my 30s. Be mindful on the timing—do not get a bone scan while pregnant or breastfeeding as this can skew the results. If you’re nursing, it’s ideal to give your body at least 6 months after weaning before you get a bone scan, so your bone health is accurate.
- Calcium & Vitamin D: People with IBD often under consume these nutrients, particularly when dairy is restricted. For most, calcium needs range from 1,000–1,500 mg/day, with vitamin D at 1,500–2,000 IU/day. In a cross-sectional study of 65 IBD outpatients, nearly two-thirds reported restricting dairy, leading to an average calcium intake of only 343 mg/day—well below the daily recommendation.
- Practical Tip: For those who tolerate dairy, start small—a dollop of yogurt, a sprinkle of cheese, or lactose-free milk. Non-dairy sources and supplements can help fill the gaps. When you get labs, you can talk with your GI about looking at your vitamin D level to see if it is adequate or not. I was on 50,000 IU once a week for many years. Now, I take 2,000 IU a day. So, this figure does fluctuate and it can improve.

Nutrition Across Life Stages
Neha stresses the importance of tailoring nutrition guidance to a woman’s age and life stage:
- Young women (around age 20): Focus on building peak bone mass, meeting calcium and vitamin D needs, and making realistic choices in dining halls or dorms. Portable, nutrient-dense snacks like yogurt, nut butter, or fortified bars can make a difference.
- Premenopausal women: Greater emphasis on long-term bone and muscle health, distributing protein intake evenly throughout the day, and pairing nutrition with weight-bearing activity to maintain strength. Neha’s focus shifts more toward optimizing long-term bone health, since risk factors may be increasing.
“Across both age groups, I prioritize adequate protein and fiber in forms that are well tolerated to help manage symptoms and optimize muscle mass, while also monitoring common nutrient deficiencies such as iron, vitamin B12, and folate,” explains Neha.
The Role of an IBD-Specialized Dietitian
A dietitian specializing in IBD plays a vital role in helping patients understand how inflammation and treatments can affect digestion, absorption, and food tolerance.
“We stay up to date with the latest evidence and tailor nutrition strategies to each stage of the disease—whether someone is newly diagnosed, recovering from surgery, or in remission. For example, we help patients identify which types and textures of fiber are best tolerated, since not all foods impact the gut the same way,” says Neha. “We also emphasize balanced protein intake from both animal and plant sources to protect muscle mass, and ensure nutrients for bone health, like calcium and vitamin D are optimized from both dairy and non-dairy options. Just as importantly, we integrate these strategies into each patient’s lifestyle, culture, and social settings so that recommendations are practical, sustainable, and supportive of long-term quality of life.”
By seeking out a registered dietitian who specializes in IBD you are truly targeting your treatment and receiving personalized care that helps you cut through the confusion, especially if you are newly diagnosed. Their strategies are not just good on paper; they work at your kitchen table and in your daily routine to help you get your health and well-being back under control.
Accessing a dietitian may depend on the healthcare system. Patients can ask their gastroenterologist for a referral, or they may be able to connect with an IBD-specialized dietitian through private practice. Many registered IBD dietitians also do virtual video calls, so it’s not necessary for in-person, local appointments. The Crohn’s & Colitis Foundation provides resources to help connect patients with dietitians who have expertise in IBD.
Final Thoughts
Nutrition in IBD isn’t one-size-fits-all. It requires careful personalization and an understanding of the unique challenges women face throughout their lives. By focusing on gut, muscle, and bone health, women with IBD can better protect their bodies today while laying the foundation for stronger health in the future. It’s not just about flares and managing our IBD, it’s about how our bodies uniquely absorb nutrients, how inflammation affects our strength, and how hormonal changes shift the way we fell over time. Muscle weakness, bone loss, and unpredictable symptoms tied to our menstrual cycles can be a lot, but small, realistic changes in how we eat and move our bodies can make a lasting difference.
Click here to learn more about Neha Shah’s work.
Connect with Neha on Instagram: @nehagastrord










