This blog was sponsored by Mahana Therapeutics. All thoughts and opinions shared are my own.
Did you know that two thirds of people with inflammatory bowel disease (IBD) also meet the criteria for a functional GI disorder? Dr. Aline Charabaty, Dr. John Damianos, and Dr. Katie Dunleavy recently presented a paper at the 2022 Guild Conference addressing the substantial overlap between Crohn’s and ulcerative colitis and the gut-brain interaction. You may wonder what constitutes a functional GI disorder, irritable bowel syndrome (IBS) is the most common.
“What we know is that up to 30-40% of patients with IBD in remission (absence of gut inflammation) continue to have GI symptoms such as abdominal pain, bloating, diarrhea, constipation, and fecal urgency, due to disorders of gut-brain interaction (DGBIs, also known as functional gastrointestinal disorders),” explained Dr. Aline Charabaty, director of the IBD Center at Sibley Memorial Hospital.

As someone who was diagnosed with Crohn’s disease more than 17 years ago, I’ve been told by multiple gastroenterologists that I have IBS as well. At one point I was told, “you have a touch of IBS” …whatever that’s supposed to mean. I know I am not alone in believing I have both IBD and IBS, especially since having 18 inches of my small intestine removed for bowel resection surgery in 2015.
Dr. Charabaty says this is the case for many patients because of the following:
- Structural damage to the gut caused by IBD. Crohn’s disease can lead to small bowel stricture, which can cause cramps and constipation (by blocking or slowing down the stool flow); Long standing UC can create a “lead pipe colon” (where the colon loses its normal twists and turns that typically slow the stool flow down and become like a straight tube which makes the stool “fall” straight down), which can cause diarrhea and urgency. Resection of part of the small bowel and colon decreases the surface of the bowel that can absorb the water and solidify stools, which leads to loose stool. Finally change in bowel anatomy from stricture or resection, abdominal adhesions from prior inflammation, abscess, or surgery, can lead to small bowel bacterial overgrowth (SIBO) which can cause bloating, pain, diarrhea, or constipation.
- People living with IBD can become intolerant to certain foods or modify their diet. This can lead to change in gut flora that affect gut functioning and lead to GI symptoms.
- Recurrent flares or previous severe inflammation can lead to change in the gut sensation. Visceral hypersensitivity, gut motility, gut microbiome, intestinal permeability, and how someone perceives and tolerates all the sensations (pain, discomfort) that come from the gut.
- IBD affects people’s emotional and mental health and is associated with a higher incidence of depression and anxiety. We know that depression and anxiety can affect the gut functioning and lead to IBS symptoms.
“All these changes are similar to what we see in people living with IBS and can cause IBS and IBS symptoms in people living with IBD. Sometimes the way I explain it to patients with IBD, is that IBS is like the PTSD of the gut. The gut has been inflamed, traumatized, manipulated, changed from prior flare and now it can’t go back to functioning properly, even if it’s healed and it looks normal,” said Dr. Charabaty.
This is where Mahana IBS comes in. The main mission? To empower people with chronic conditions to lead fuller lives through digital therapeutics. That’s why they debuted their new prescription digital therapeutic app, Mahana IBS, in the fall of 2021. Their wish is to destigmatize IBS and bring hope and meaningful solutions to patients like you and me.
Steven Basta is the CEO of Mahana Therapeutics. He says the app is safe, FDA-cleared, and has been clinically proven in the world’s largest trial of its kind to reduce IBS symptom severity.

“Cognitive Behavioral Therapy (CBT) has long been recommended in clinical guidelines as a safe and effective treatment for IBS. Access to traditional CBT with a therapist has been a huge challenge due to the limited number of IBS-trained therapists (less than 300 in the US). Now patients can access CBT and learn the skills it provides to help a patient manage their disease by using Mahana IBS on their smartphone, with great results: 3 out of 4 patients find relief and results for most patients are lasting. Mahana users can complete the program in 90 days or less at their own pace with daily lessons on their phone to create a healthy brain-gut connection and live life more fully.”
Both IBD and IBS negatively impact our quality of life. Our mental health, our psychosocial health, and our financial health (increased health care utilization, missing days of work, medications to treat symptoms).
“Beyond treating the inflammation of IBD, and preventing IBD-associated complications, it is important to recognize and treat IBS when it is present, so people can recover and optimize their quality of life. CBT is an effective therapy for IBS and reduces or eliminates symptoms of abdominal pain, diarrhea, constipation, and bloating,” said Dr. Charabaty.

Unfortunately, access to a therapist who can provide gut-directed CBT can be limited: lack of therapists trained in CBT in someone’s geographical area, limited time availability (many therapists are not taking new patients, or have long waits to see someone; or from an IBD patients’ standpoint—lack of “extra” health care time available, when we often juggle many health appointments), deal with lack of insurance coverage, additional costs related to taking time off work and the expenses related to travel and participate in CBT sessions. Which makes the app even more useful and beneficial for the patient community.
Bringing up digital therapy to your GI provider
Digital therapy is new, and Mahana Therapeutics is working hard to spread awareness in the clinical and patient community to ensure everyone who could benefit, has access, and knows about Mahana IBS.

“It’s important for patients living with IBD to ask their doctor whether Mahana IBS is suitable for them and discuss how it can work with their treatment plan,” said Steve.
As a gastroenterologist who specializes in IBD, Dr. Charabaty says, “Having an FDA-cleared prescription app that provides CBT right at the patient’s fingertips is pure gold! Easy and effective access to CBT at a time that is convenient for the patient, in the privacy of their home, without the added extra time and cost burden of a visit to a clinician. I believe that with this technology/app, which removes many barriers to accessing therapy for IBS, that many more people living with IBS (whether they have IBD or not) will benefit from what CBT has to offer and will be able to improve their symptoms and regain their quality of life.”
Patients who are in IBD remission experiencing IBS Symptoms may want to ask:
“If my IBD is in remission and my symptoms are IBS related, could a digital therapy treatment such as Mahana IBS gut-directed CBT be suitable for me?”
GIs who want to understand more about the clinical evidence and indications for use for Mahana IBS can head this website to check out the medical provider welcome pack which contains all the clinical information they need to get started and to prescribe Mahana IBS.
While the app is a prescription, patients can also download the app on their own and show their gastroenterologist in clinic. But to gain access to the full program, patients need to get a prescription to unlock the benefits.
How the app is tailored to each patient
People experience IBS differently which is why Mahana IBS provides a personalized approach, regardless of type of IBS. In the early sessions of the app, patients create an IBS symptoms profile, take an IBS Symptom Severity Score assessment, and create their personalized model.
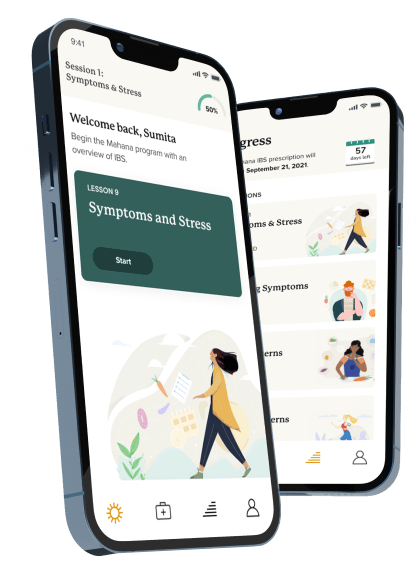
“This means people get to identify and capture their own symptoms and associated thoughts, behaviors and actions that arise as a result of these. As patients progress through the app and unlock tools and content, exercises are provided that are tailored to people’s individual IBS symptoms. Progress is recorded through the IBS Symptoms Severity Score at the beginning, the middle, and at the end of the program to measure results,” explained Steven.
Reframing thought process to reduce IBS symptoms
We can all relate to how feeling anxious can leave our ‘stomach in knots’ but in IBS there is a disorder of the brain-gut communication which causes and perpetuates symptoms. For example, our guts can release hormones that change our mood, and the brain in turn sends a signal to our guts to change our bowel functions which then sends more signals to the brain.
“Patients may develop habits or use ‘coping’ techniques that perpetuate the vicious cycle of brain-gut miscommunication without knowing it. The Mahana IBS app uses a gut-directed CBT program that was researched and developed over several decades. It is designed so you can understand your personalized patterns and then learn skills to help support a healthier brain-gut interaction. The program delivers a combination of education and exercises so that patients identify and reframe thoughts, feelings, and actions related to IBS. Through the Mahana IBS program, patients can gain tools and habits for managing symptoms long-term,” said Steven.
Along with learning to reframe our thoughts, the app also features visceral relaxation exercises like diaphragmatic breathing or belly breathing, which can reduce visceral pain and improve GI function. Mahana IBS has easy to follow animations to help patients learn and practice these techniques.
While Mahana IBS is a treatment program designed to be completed in 90 days or less with lasting results, Steve tells me some patients may experience relief from their functional GI disorder within a matter of weeks.
“Patients go at their own pace, so they may complete the program more quickly. Once the 90 days have elapsed, patients can still access their personal data (for example goal setting, IBS-SSS score or their personal IBS Model). Patients can return to the app at any time to find support in any of the lessons, tools, and exercises they have completed.”
Accessing Mahana IBS
Mahana is committed to affordable access. Some patients may be reimbursed by insurance. For those patients who are not covered by insurance, there is a subsidized program to ensure patients will pay no more than $90 out of pocket for prescription cost. That’s less than a single session with a therapist ($120/session) for the complete 10-session program.
Steven says it’s incredibly rewarding and a huge privilege to lead the Mahana team transforming access to treatments like this through digital therapy.
“As CEO of Mahana Therapeutics I am inspired by so many amazing patients with IBS. One patient who had struggled for years with IBS symptoms that made her feel truly hopeless expressed that Mahana IBS changed her life. With the lessons and skills she learned, she no longer avoids the food she loves, and the way she thinks about IBS has altered so completely, it no longer limits her life. Our team’s mission is to make this story a reality for millions of IBS patients.”
Mahana IBS is available for download directly from the Apple App store and Google Play store—and the first session is free to try! To unlock all the specific features and benefits, you’ll want to get a prescription from your GI. Once you’ve been prescribed the app by your doctor, you will get a message from Blink Pharmacy with instructions to get started.




