It feels like a punch to the gut. Even though you’re anticipating it, the experience is not easy for anyone. For patients with inflammatory bowel disease (IBD), stability is everything. Whether living with Crohn’s disease or ulcerative colitis, finding a medication that keeps symptoms under control is often the result of years of trial and error. So, when insurance companies or healthcare systems mandate a switch from a familiar biologic like Humira to a biosimilar such as Hyrimoz or Amjevita, the decision can feel sudden, confusing, and unsettling. As of right now (May 2025) there are 22 FDA-approved biosimilars on the market for infliximab (Remicade), adalimumab (Humira), and Ustekinumab (Stelara) with many more coming down the pipeline.
It’s easy for providers to rely solely on the science that says it should be a “seamless,” effortless transition for patients and caregivers—but that’s not always the case, nor is it ever a guarantee. This week on Lights, Camera, Crohn’s we hear from more than 30 patients who have lived this reality. While many people seem to do well clinically, it’s imperative that we also discuss the mental and emotional toll this forced non-medical switch takes on people with chronic, debilitating illnesses and their caregivers. This blog aims to demystify biosimilars, highlight the emotional and clinical complexity of switching therapies, and provide guidance for healthcare providers and patients navigating this challenging transition.

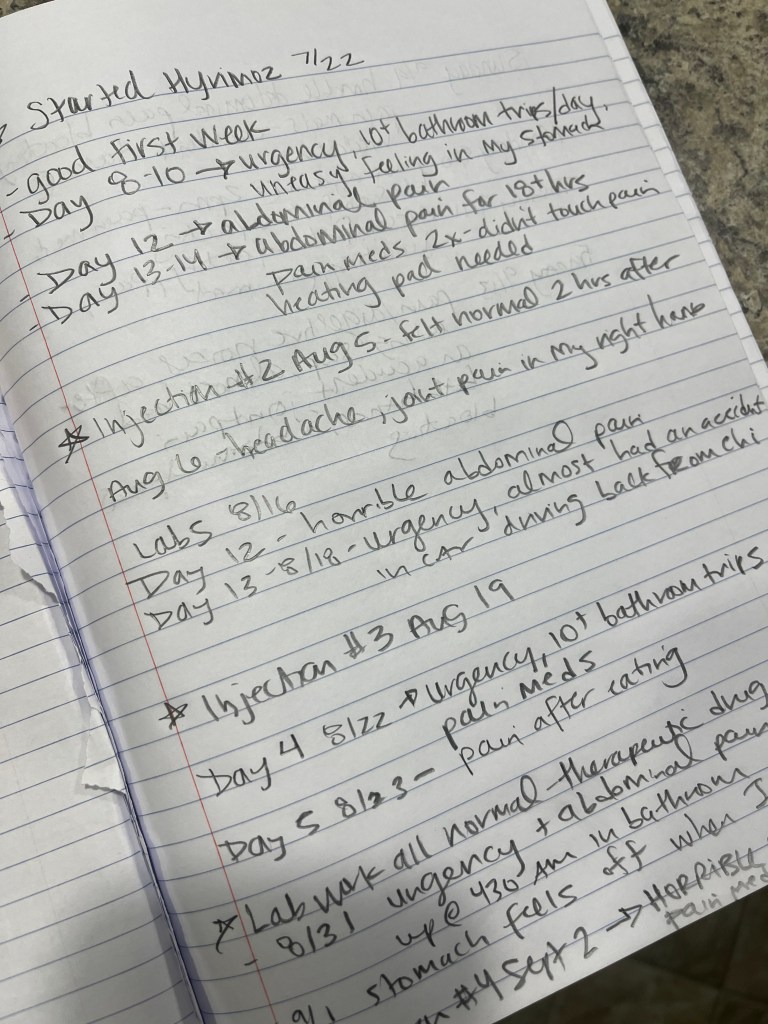
As someone who was forced off my Humira after being on it for 16 years and put on Hyrimoz, I empathize with how complicated this is for patients. Not only was I petrified to switch—but I had a God-awful experience that resulted in going from deep remission to dealing with an adverse response for two months of my life, while trying to be a mom to three young kids.
I don’t take this subject lightly and frankly; I don’t care who I piss off by sharing this patient experience transparently. I angered some donors from a Pharmacy Benefit Manager (PBM) when I spoke on stage in front of a large crowd last fall genuinely thanking my IBD nurse who went to bat for me countless times to help me win my appeal to get back on Humira—this isn’t about profit, it’s about patients. We don’t owe anyone an apology for being uncertain about being told we need to switch our heavy-duty drug therapy not by a doctor, but by someone working in corporate America.
Biosimilars are not generics
First things first, I must clear the air on this. Almost every direct message I receive from patients refers to biosimilars as “generics” …and that’s a common misconception that needs to be done away with.
Unlike generic drugs, which have identical active components, biosimilars are comparable but not identical to their originator drugs. According to the US-FDA, a biosimilar is a biological product that is potent, pure, and safe and that is “highly similar to and has no clinically meaningful differences from an existing US-FDA-approved reference product”. In other words, biosimilars are equivalent to the reference biologics regarding safety and efficacy.

When you hear the terms “originator” or “reference” biologics—that means Infliximab (Remicade), adalimumab (Humira), and Ustekinumab (Stelara). There are many other biologics of course, but so far, these three biologics have biosimilars approved by the FDA. You can familiarize with their names that I’ve listed below so if you see one listed in a letter it’s not foreign to you.
Infliximab Biosimilars:
- Inflectra (infliximab-dyyb)
- Renflexis (infliximab-abda)
- Avsola (infliximab-axxq)
- Ixifi (infliximab-qbtx)
- Zymfentra (infliximab-dyyb)
Adalimumab Biosimilars:
- Amjevita (adalimumab-atto)
- Cyltezo (adalimumab-adbm)
- Abrilada (adalimumab-afzb)
- Hadlima (adalimumab-bwwd)
- Hulio (adalimumab-fkjp)
- Hyrimoz (adalimumab-adaz)
- Idacio (adalimumab-aacf)
- Yuflyma (adalimumab-aaty)
- Yusimry (adalimumab-aqvh)
- Simlandi (adalimumab-ryvk)
Ustekinumab Biosimilars:
- Wezlana (ustekinumab-auub)
- Selarsdi (ustekinumab-aekn)
- Otulfi (ustekinumab-aauz)
- Imuldosa (ustekinumab-srlf)
- Yesintek (ustekinumab-kfce)
- Pyzchiva (ustekinumab-ttwe)
- Steqeyma (ustekinumab-stba)
Important note: While these biosimilars have received FDA approval, the availability of some may be subject to patent litigation settlements or market launch agreements, potentially delaying their commercial availability.
Let’s look at the real-life numbers
While working on this article, I ran several polls on Instagram asking the IBD community about their personal experiences. Some of the findings surprised me:
Have you received a letter saying you have to switch? Of the 265 respondents, 64% of patients said “yes”, and 36% said “no”.
Did you appeal before switching to a biosimilar? Out of 200 responses, 33% responded “yes” and 67% responded “no”.
For those who switched was the transition seamless—or did you notice an uptick in symptoms? Of the 140 responses, 51% had a seamless transition and 49% noticed an uptick in symptoms. This right here speaks volumes.
If you responded poorly to your biosimilar and your GI appealed insurance, what was the outcome of the appeal? Out of 75 responses—38% of patients were denied, 32% were put back on the originator drug (biologic), and for 30% after multiple appeals they finally won and returned on their biologic.
Let’s hear directly from patients
Bre: “I was taken off Humira after the New Year and placed on Simlandi for my ulcerative colitis. I was nervous as I had just come out of a two-year flare and had finally found a drug that worked and even though I was reassured that this was as good as Humira, I still had my doubts. Thankfully, I have had a positive experience and have remained in remission since starting Simlandi in January. I hope this story helps others feel less afraid of the potential outcomes when they get the dreaded non-coverage letters.”
Kyrsten: “Back in April I was forced off Stelara to the biosimilar, Yesintek. I went into it with an open mind because my Crohn’s has been in remission for about a year and a half. Unfortunately, I am now experiencing more symptoms that I’m documenting and oral manifestations of Crohn’s and need to see an oral medicine doctor now.”
Stefanie: “I’ve had to switch biosimilars twice at this point, this second time, while I was pregnant. I’m doing just fine!”
Alexandra: “I was first afraid of Humira, then I grew into being afraid of not having it; so, when my insurance mandated the switch to Hyrimoz late last summer, I was so worried (as all are/were)! In September, I was starting to feel some symptoms pop in, so we did all the tests, which indicated that I was still in clinical remission. Thankfully, I am doing ok now with no issues.”
Christina: “It was first recommended to me by my GI a couple of months after diagnosis in 2021 to start on biologics, since the oral medications had stopped working for me. We collectively decided the best option for me would be Remicade, however when it was brought to my insurance company, they immediately denied it. Insurance said it wasn’t their “preferred method” and wanted me to try and fail Humira first. When my GI tried to get the Humira approved, my insurance company ended up denying that, too, and this time, their excuse was it “wasn’t medically necessary.” It took my GI a couple of months to get a biologic approved and I almost ended up back in the hospital as a result.”
After receiving her first injection, Christina ended up developing an allergic reaction and had to be switched to something else. After another month of fighting insurance, Christina’s GI was able to get Remicade approved.
Christina goes on to say, “I did very well on that for about a year, until my body developed antibodies, and I had to switch once again. I then started Entyvio infusions which I have been on ever since, and so far, I’ve been doing well on it.”
Audrey: “I was forced to switch from Remicade to Inflectra a few years ago due to insurance coverage. My job at the time was horribly stressful and very time-consuming and getting the news then about my medication no longer being covered and that my next infusion was delayed because of this change over the phone from my infusion clinic was terrible. I remember sitting in the workplace cafeteria when my phone rang, and I burst into tears and was pleading with the pharmacist that gave me the news prior to receiving the letter.”
At this point, Audrey was receiving Remicade every seven weeks. With the delay and having to wait for Inflectra to be shipped, she was pushed out an extra week.
“The thing that made me so angry, was that I had already received my Remicade shipment, the nurses just weren’t allowed to mix and dispense it because of the insurance change. I refused to toss that Remicade dose until the vials expired, since I knew how costly it was. I called so many charity pharmacies for low-income folks to see if they could take the vials and since its temperature controlled, they couldn’t. Such a waste,” said Audrey.
Thankfully, Audrey tells me she hasn’t had any issues with the switch, and she’s stayed in remission—even during and after her first pregnancy. But she says the stress and frustration that occurred impacted her mental health at the time.
Kelly: “I just got the letter. Been on Stelara since 2017. I also take it every four weeks, even though the recommended dose is every eight weeks. I get my insurance through my husband and our insurance turns over on 6/31/25. The new policy begins July 1st. I’m really concerned and honestly don’t want to deal with this.”
Sandi: “I was forced to change from Remicade that had me in remission for several years to Inflectra and the outcome was not good. I had multiple Crohn’s flares a month, which was not happening when I was in remission. My GI appealed and after a year, insurance started to cover my Remicade again. Since getting back on Remicade, I’m in deep remission, again.”
Britt: “I was diagnosed with Crohn’s in 2011 at the same time I was diagnosed with Primary Sclerosing Cholangitis (PSC), a rare liver disease. I was on Remicade and was switched to Avsola. For a while, I was quite skeptical, but we stayed the course. I had some ups and downs with my health, but I was just told I am in histological remission by my GI! After five years of struggles to find the right medication, my health finally seems to have aligned. I also take 6mp to reduce antibody development to the Avsola.
Danielle: “I went into my pregnancy in remission and my first and second trimesters were lovely. About halfway through my pregnancy, insurance decided it was the right time to swap my medications. Two weeks following that change, I was already struggling. I ended up finishing my pregnancy on two different rounds of methotrexate and iron infusions. I had a scheduled C-section at 39 weeks, and I think my care team hoped that my body was just struggling balancing pregnancy and Crohn’s…that was not the case at all.”
Danielle says she tried two more Inflectra infusions after her daughter was born and saw no improvement. She required a round of prednisone and that didn’t help either. She was then switched to Humira injections every two weeks and they seemed to work wonderfully and she started to feel better.
“Then my insurance threatened to switch me to a Humira biosimilar, but Humira failed me right when that was supposed to happen, so I was transitioned to Entyvio. For six months I saw no improvement on Entyvio…more prednisone and still NO improvement. Finally when my daughter was 14 months old (so over a year and a half of feeling like absolute garbage and having no energy) I got bowel resection surgery and switched to Stelara.”
Danielle went on to say she’s been in remission since December 2021, and she still wonders if switching to the Remicade biosimilar caused all this to happen.
“I truly feel like that change took part of the joy of pregnancy away from me and also took a lot of special time away from my daughter the first 14 months of her life. I spent her second Christmas in the hospital unable to see her for two weeks. I was on so many pain medications for so long before the surgery that I don’t remember her first birthday. I lost a lot simply because someone was trying to cut costs and making decisions they are not educated about.”
Brooke: “I was on Remicade for 15 years, then I was forced to switch to Inflectra. I was incredibly stressed and tried to appeal but lost that battle. I’ve now been on Inflectra for 3 years and I am doing well! I still hate that we are forced to change when something is going well. The amount of stress, anxiety, and time I spent fighting the insurance company took a toll on me.”
Brooke went on to say that she got pregnant and had a daughter while on Inflectra. Her GI and OB had no concerns with the biosimilar during pregnancy.
Maya: “At the beginning of March, I was told by my insurance that Stelara will no longer be covered and that I would be put on Yesintek. I’ve only gotten one dose of it so far, but I very much empathize with all the emotions that come with getting the letter. So far, I haven’t noticed any additional symptoms or changes in how I feel. I’m hoping Yesintek works for me and that I continue to feel ok!”
Maria: “I live in Sweden where Humira is covered by the State since no private insurance is needed, the last year though I was recommended from doctors to switch to a biosimilar. So, in autumn of last year, I decided to try Hyrimoz. I noticed no difference in the first three months, but after that, I saw an increase in symptoms, especially for my rheumatoid arthritis. My doctor recommended that I take the injection weekly instead of biweekly, but that didn’t help at all. Since I haven’t developed any antibodies, my doctor switched me back to Humira and I felt the difference right away.”
Sadly, Maria recently got the news that Humira will no longer be covered in Sweden starting in August, so she will either have to pay out of pocket or find another medication.
“You can imagine how that feels. Humira has been my trusted friend since 2008, managing my Crohn’s and RA so well. Hard to think of life without it,” Maria said with a tearful emoji.
Kenzie: “I’ve been on two different biosimilars of Remicade. Inflectra was seamless—no issues. Then, a few years later, I got new insurance, and they made me switch to Avsola, which I had an allergic reaction to. No allergic reactions to Remicade or Inflectra, after being on them for more than six years. Now I’m on Cimzia injections (not a biosimilar) because it’s safe for nursing and that just seemed like the better option for me right now. I’ve only been on Cimzia for 10 weeks, but so far, my Crohn’s and RA seem slightly better.”
Audrey: “I switched to a biosimilar (Inflectra) in January 2022. I got pregnant in June 2024 and delivered a healthy baby boy this March. No disease issues thus far.”
Tara: “I was on a biosimilar when I conceived and throughout my entire pregnancy. I’m on Hulio and everything went well. I stayed in remission throughout the pregnancy and postpartum.”
Amanda: “I was able to conceive and am currently pregnant on a biosimilar. Everything is going great, thankfully I was on Humira for about six years and then got the dreaded letter to switch. I went on Hyrimoz at the end of last summer and was on it for five months prior to getting pregnant.”
Lauren: “I conceived and was pregnant with my now 3-week-old all while on Inflectra. I stayed in remission the whole time.”
Katie: “I was able to conceive while on Avsola, a biosimilar to Remicade. I haven’t experienced any issues related to pregnancy. I did develop some antibodies though and had to escalate my dose while pregnant. I also take premeds of Solumedrol and Benadryl before every infusion now. I got hives during the Avsola infusion while I was pregnant.”
Erica: “My doctor wouldn’t appeal it. I was put on Amjevita. Thank goodness and knock on alllll the wood…it’s been going well. I haven’t noticed any difference in symptoms. It’s been a little over a month, so I pray it stays that way.”
Jessica: “Conceived and pregnant on Inflectra infusions. I just had a healthy baby girl one month ago, and I’m now breastfeeding. No problems at all.”
Marla: “I switched to Hyrimoz while pregnant and I did not notice a change. However, I will say I’ve been in remission since getting pregnant with my first child and I don’t always take my medicine on time, so I don’t know if the transition was seamless because the medicine is truly fine or if it’s because my body just does well while I’m pregnant and breastfeeding (which I basically have been the past four years having three babies). I will say it’s an ABSOLUTE nightmare trying to get my medication each month. Constant bills I’m having to fight and constant new prescriptions and prior auths from my doctor for the SAME medication. It’s literally unreal. I blame that on CVS Specialty pharmacy.”
Amanda: “While I was pregnant, my OB appealed because insurance would no longer cover my Delzicol for ulcerative colitis. I won but was only allowed to stay on it until I delivered, then I had to switch to a generic mesalamine.”
Christine: “Pregnancy is what got me a temporary appeal. Once the baby was born, I had to switch, but it was peace of mind not having to make the transition during pregnancy. I was anxious that it was just a regular infusion, there wasn’t a loading dose or a slow rate or anything. They just infused the Inflectra the same way they infused the Infliximab. About two years after making the switch, I had to go from every 7 weeks to every 6, but I will never know if it was due to the biosimilar or if after 10 years on a biologic/biosimilar, my body just needed the drug at more regular intervals.”
Danielle: “I was pregnant (in remission), and my GI decided that was the correct time to switch me to Inflectra from Remicade…it did NOT go well.”
Jordyn: “I found out I was pregnant around the same time I had my first biosimilar infusion. I went through my whole pregnancy on the biosimilar and only noticed an uptick in symptoms around 10ish weeks, which a course of steroid foam resolved. Postpartum is when I noticed the return of symptoms the most. After 2 or 3 infusions (I get them every 4 weeks) with no improvement, I asked for an appeal, and it was granted for me to go back on Remicade.”
Natalie: “I got pregnant the month after switching to Avsola. I made the switch November 2022 to the biosimilar and found out I was pregnant December 29th. Pregnancy went fine, delivered in August 2023, all my problems started in February 2024. I went back on Remicade at that point because my GI suspected I had serum sickness for months on end, and to this day, they still aren’t sure if the serum sickness initiated my problem of Crohn’s attacking my joints.”
Angie: “We were told we would have to switch, but the doctor office contacted them, and they will be covering me at least until September for Humira…then we will renew the prescription and hope that it will be covered, again.”
Jasmine: “I’m on Avsola (biosimilar for Remicade) and I wasn’t trying to get pregnant, but did, and had a perfectly healthy pregnancy.”
Allie: “My specialists appealed saying I was going through fertility treatments and then insurance approved my Remicade for another year.”
Malea: “I got my insurance letter recently and have been meaning to reach out as I remember your Humira nightmare. I have not appealed yet, partly because my GI office is incredibly dysfunctional and hard to get ahold of. I am on Stelara, which is the first thing to have kept my Crohn’s in remission and they want me to switch to Selarsdi, which I can not find any patient experiences/anecdotal evidence about.”
Georgia: “I was on Humira last summer when Accredo tried to switch me to a biosimilar without notification. I had a letter saying that my Humira was still covered. I worked with my GI who told me they are seeing this a lot and if the person doesn’t push back, they just switch them to a biosimilar. But, if the person pushes back, the GI calls Accredo with a code (DW1 Brand Medically Necessary) to block it. That’s what I did, and they therefore had to send me my Humira since my insurance was still covering it. I want to let others know in case they have a prior authorization from their insurance saying they will cover Humira, despite the pharmacy trying to switch them!”
Jessica: “I so appreciate you talking about this. For my daughter, I went to refill her Humira, and insurance said the doctor allowed the switch. I asked the doctor, and they said no…it’s insurance. I had to use one of my daughter’s biosimilar pens while mine was being shipped, and I noticed more pain and burning. I advocated for my daughter to be on brand name only and they approved the request. When it came to my biologic, my letter had the same wording and once again it was insurance, not my doctor.”
Jessica’s GI said despite her being in remission for so long, she would need to try the biosimilar, then if any symptoms occurred then they could fight for return to the originator drug.
The Emotional Toll of a Forced Switch
For many patients, switching medications, especially after long-term remission, can trigger anxiety, mistrust, and a profound sense of vulnerability. Here are a few of the emotional and psychological responses patients may face:
- Fear of Flare-ups: Patients often fear that a new medication might not work as well, risking disease recurrence and potentially hospitalization. So many of us have been relying on our biologic as a crutch for several years if not decades, it’s worrisome when you find a medication that works and have to change simply because insurance decides it’s necessary.
- Loss of Control: Being told to switch due to non-medical reasons (like insurance mandates) can feel disempowering.
- Medical Trauma: Those who’ve experienced years of instability before finding an effective treatment may associate medication changes with setbacks and suffering.
- Distrust in the System: Patients may feel like financial decisions are being prioritized over their health and well-being.

How to Comfort and Support Patients Through the Transition
Healthcare providers and care teams play a critical role in guiding patients through these difficult changes. Here are some key strategies to help:
- Educate With Compassion: Clearly explain what biosimilars are, how they’re tested, and what the current evidence says about their safety and effectiveness in IBD. Emphasize that switching is based on clinical research and real-world data, not just cost. Have discussions about biosimilars with patients in clinic even if they haven’t received a letter in the mail yet so they are prepared.
- Validate Their Concerns: Avoid minimizing fears. Instead, acknowledge them openly. Saying, “I understand why you’re anxious about this” creates space for honest discussion and trust-building.
- Monitor Closely After the Switch: Set up a proactive monitoring plan to track disease activity, symptoms, and lab markers. This can reassure patients that you’re watching for any changes closely—and are ready to act quickly if needed. As a patient leader who unfortunately had to appeal my biosimilar, the fact I kept a detailed journal for two months and then wrote my own appeal letter in conjunction with my GI really helped us win the appeal.
- Advocate When Necessary: If a patient is stable and deeply concerned about switching, advocate on their behalf. Some payers allow exemptions if a provider makes a strong clinical case for staying on the original biologic. It may take extra paperwork, but the effort can mean everything to the patient, especially for pediatric patients and women who have family planning considerations.
- Encourage Peer Support: Connecting patients with others who have made similar transitions can provide reassurance and reduce feelings of isolation. Patient communities, both online and in-person, can be powerful.
Navigating the Complexity of Informed Consent
True informed consent means patients understand not just the science, but the context of their decision. It’s more than ticking a box—it’s about creating space for dialogue, questions, and partnership. When I received the letter saying Humira would no longer be covered, I alerted my GI team not to sign the new script, as that gives the pharmacy/insurance the ability to switch you. A biosimilar is not able to be prescribed until your doctor signs off on it, remember that.

A thoughtful approach might involve:
- Discuss what will happen if symptoms worsen after switching. My GI called me multiple times to comfort me and even prescribed a couple of Xanax pills to ease my anxiety leading up to the switch.
- Review the process for switching back (if possible). Have a game plan in place so you’re not scrambling if you notice a change in your health.
- Ensure patients know they won’t be left to manage complications alone. Support every step of the way makes all the difference.
Research articles to help you feel informed about biosimilars
An informed patient is an empowered patient. I did some research to help do the homework for you. By reading the articles below you should feel better educated on biosimilars so you feel more comfortable with the switch (if it’s a necessity) and about discussing this further with your care team:
Biosimilars in IBD Treatment: Expert Panel Discussion | IBD Pro
Biosimilars in Pediatric IBD: Updated Considerations for Disease Management – PMC
Biobetters and biosimilars in inflammatory bowel disease – ScienceDirect
Biosimilars in IBD: What Every Clinician Needs to Know – PubMed
When to Switch Biosimilars for Patients with Inflammatory Bowel Disease
Biosimilars Gastroenterology Roundup: March 2025
Final thoughts
Switching from a biologic to a biosimilar can feel like stepping into the unknown—but it doesn’t have to be done in fear or isolation. With transparency, empathy, and collaboration, patients can be empowered to make informed decisions, feel supported during the process, and maintain confidence in their care.

While some people feel more confident switching from a biologic to a different drug class (for example, Humira to Skyrizi or Stelara to Entyvio) to dodge the biosimilar, others are fearful of building up antibodies to a drug class that is otherwise working. You must weigh the pros and cons and do what you feel most comfortable doing. It’s important to remember it’s only a matter of time until all biologics for IBD have biosimilars, so by switching drug classes you are most likely just delaying the inevitable.
If you are planning to become pregnant or you are currently pregnant and on a biologic or a biosimilar please check out the PIANO registry so you can help pave the way for future IBD families and contribute to research so we have more information about the safety of these medications in pregnancy.
The science behind biosimilars is promising. But the human side of medicine—the fear, uncertainty, and trust involved in change, must be just as carefully managed. I hope after reading this article you feel less alone and supported in your personal health decisions.