It’s no surprise Inflammatory Bowel Disease can wreak havoc on more than just our guts. And dental health is no exception since it’s technically part of the digestive tract. I’ve had Crohn’s disease for nearly 19 years, and luckily, I feel my teeth and mouth have been mostly unaffected up until recently. That’s not the case for many in our community though. I ran an Instagram poll and asked, “Do you feel your IBD impacts your dental health?” Of the 372 people who responded, 51% said “yes”, 23% said “no”, and 26% were unsure.
To provide a little backstory on my personal situation, when I was pregnant with Reid (my oldest) in 2017, I developed an abscess on my molar that went away once he was born, so luckily no medical intervention was needed. And then, when I had COVID for the first time in January 2021 I started experiencing pain in that same upper molar. It’s been two years now, and after several visits to the dentist to investigate it further, we were never able to get to the root of the problem. The pain would come and go, so we just kept a close eye on it. A root canal felt like a last resort, and I didn’t want to do anything that drastic until absolutely necessary, so I kept choosing the conservative route.
Fast forward to December 30th, 2023. The pain came back with a vengeance. I randomly was directly exposed to COVID the day before but didn’t get the virus. I found it interesting that the pain began almost immediately after the exposure though. After the New Year, I went to the dentist and found out there was a lesion on one of the roots of my upper molars and a root canal and crown were needed. The pain was unbearable, but antibiotics (a Z-pack) helped get the pain under control after about five days. While I dreaded getting all this dental work, I’m ready to be able to eat on the left side of my mouth again after two years of avoiding it and not having any pain in my mouth.
This week on Lights, Camera, Crohn’s a deep dive into dental health and how it relates to our IBD. Some people with Crohn’s and ulcerative colitis deal with ulcers and inflammation in their gums, and then the medications we take and the malabsorption we deal with can cause our tooth health to be subpar.

Oral health and IBD
According to a study entitled, Oral Manifestations of Crohn’s Disease: A Systematic Review – PMC (nih.gov), ulcers, gingivitis, and angular cheilitis are the most frequent dental issues those with Crohn’s disease experience. This systemic review concluded that, “Some lesions develop silently and go unnoticed by the patient. Others become established, causing pain, and incapacitating the patient in their normal life, sometimes accompanied by gastrointestinal symptoms.”
A study, entitled, “Dental and periodontal disease in patients with inflammatory bowel disease” also investigated how IBD can manifest orally in patients. This looked at DMFT (Decayed, Missing, Filled Teeth) scores and looked at the electronic health records of 229 IBD patients in comparison to non-IBD patients. The results showed “Crohn’s disease patients have significantly more dental health problems compared to the control group.”
With my root canal this past week, the inflammation was so out of control it required three shots to the roof of my mouth, two in the side gum area, and a burst of prednisone after. As a veteran IBD patient, I feel anytime something with my health goes awry, I immediately wonder if there’s a correlation to my Crohn’s. It’s hard not to.

This study found that people with IBD are at an increased risk of developing cavities and oral infections and that people with IBD have more dental treatments than those without IBD.
Lifestyle and dental health
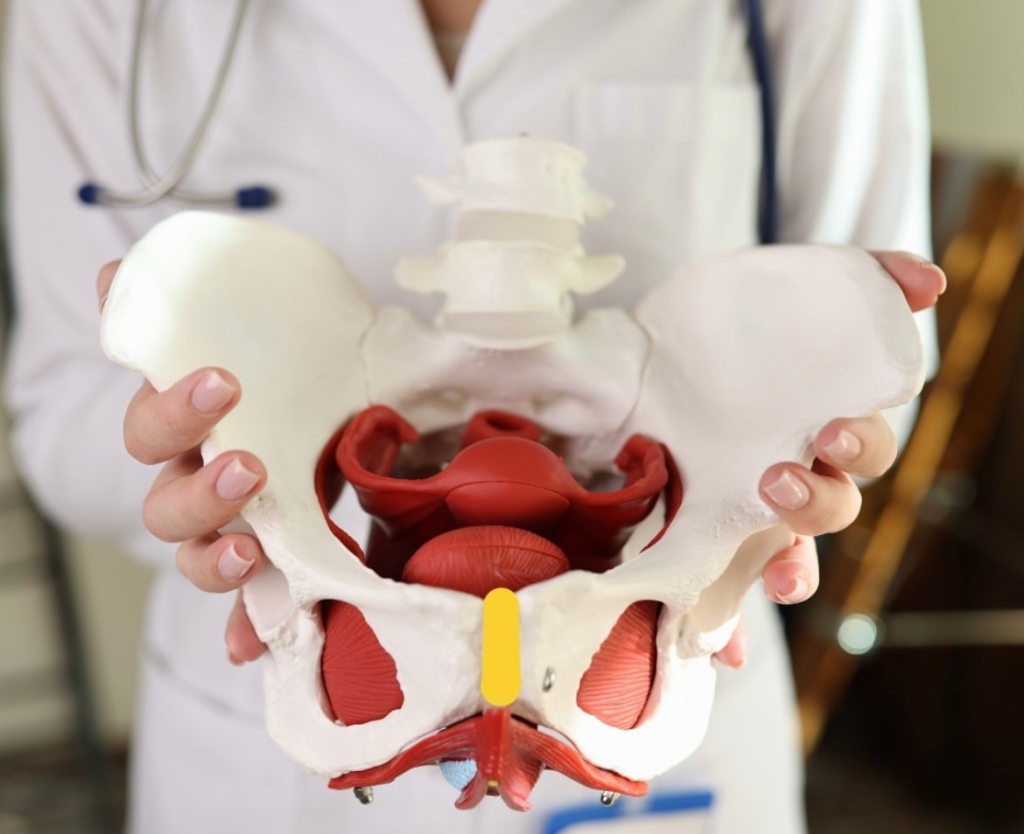
How healthy our mouths are can also directly help or hurt how our IBD manifests. Recent research in the journal Cell showed that periodontitis, or gum disease, aggravates gut inflammation because the bad bacteria in the oral cavity migrates to the gut.
Steroids like prednisone can cause loss of calcium from our bones and lead to osteoporosis, this can also reduce the calcium in our teeth, causing them to weaken and decay. Talk with your GI and make sure you are getting enough calcium in your diet to keep not only your bones, but your teeth strong. Just this week, my GI advised I chew two Tums a day for added calcium, so I’ve added that to my Crohn’s management regiment.
People with IBD sometimes struggle to find foods they can tolerate—which can result in a high sugar diet or a low amount of essential nutrients. Teeth are affected by both. Some of us also deal with stomach acid and bile coming up through our mouths. An extra acidic mouth can be caused by poor gut health. Fruit juices, fizzy drinks, and pop/soda can increase the amount of acid in our mouths. Too much acid can cause tooth enamel to erode and makes our mouths the perfect breeding place for plaque (bacteria which can cause gum disease) and gingivitis (inflammation of the gums).
What patients have to say
“I’ve had so many root canals and crowns. Last spring, I had a molar pulled for an implant. The pain with a root canal is EXCRUCIATING!”
“A little bit of clove oil essential oil placed on a Q-Tip on the area helps. Typically, IBD patients are not supposed to take ibuprofen. But I have found three ibuprofen helps a bit, too temporarily.”
“Try swishing coconut oil.”
“I had two cavities in the last week. I never had dental issues before my ulcerative colitis.”
“I’ve had three molars fixed now, either via extraction or root canal and crown. I have one more molar that needs attention because it broke (thankfully didn’t expose a nerve or anything, so it’s hasn’t been painful). The pain before surgery with the others was unbearable! I did warm saltwater rinses and ate as many cold things as I could.”
“I’m a dental hygienist and a Crohn’s patient. You should be on antibiotics and should have pain meds. Find a new dentist if they don’t offer these options.”
“Tylenol and Ibuprofen cocktail! Works like Vicodin without the woo woo effect. 800 mg ibuprofen and 600 mg Tylenol, every 6 hours. The actual procedure itself is a drop in the bucket compared to what we go through.”
“INSIST on oral antibiotics after. Even if your dentist swears you don’t need them. Speaking from experience with a dentist who wouldn’t prescribe after a root canal while on Humira. Ended up in the emergency room with a massive abscess, and many further dental issues that resulted from that infection including a re-treatment of the tooth, cellulitis, and eventually oral surgery and an extraction.”
“There is nothing worse! This is such an overlooked topic in both the IBD and dental worlds! I have serious traumas about dental procedures due to the lack of knowledge in the dental industry. I’ve been told there’s no gluten in cleaning abrasives (there was), I’ve been told that I have poor hygiene, that I’m a bad example to my kids, that I’m lying to the dentist about my teeth care. I’ve been left in pain repeatedly from neglect, and I’ve switched dentist offices about 2 dozen times. It’s been a battle!”
“It’s the worst pain. They wanted me to wait for a root canal until after my wedding and honeymoon and I cracked, and had it done a few hours before my rehearsal dinner because I would not have enjoyed my wedding. I felt like a MILLION bucks after even though it still hurt. It’s not the type of pain you can ignore.”
“My gums always bleed, and I constantly used to get told at the dentist that I must not floss or brush daily. Not true. It drove me nuts. I would brush my gums so hard thinking that eventually they would stop bleeding for the next appointment at the dentist. This only caused receding gums. I told this to my new dentist and his staff, and they don’t say anything about my gums bleeding.”
“I have ulcerative colitis and had a root canal and crown 10 years ago; it was a great success. I never had any more issues. I had such a tough time finding antibiotics that helped. So, they gave me penicillin and that exacerbated my symptoms of UC.”
“Our teeth are a hot mess due to IBD and more specifically long periods of prednisone.”
“I had to get an emergency root canal while pregnant, so we had to limit anesthesia during the process. I would not recommend this. The process wasn’t great but wasn’t the worst considering Crohn’s and birth pain. One takeaway would be to know your gums might flare back up for a few months afterwards. As a mom with Crohn’s and gum disease, I would love to see a piece on IBD an dental health.”
“I would just have the tooth pulled personally. It can end up having an infection and you won’t know because the nerves are gone, and your teeth are connected to your whole body. There’s even a movie about it. Hypericum homeopathy would be great for nerve pain. You could rotate that with arnica every two hours. I would also place a clove in a little cotton and set it back there or clove essential oils in coconut oil and rub it around the gums in that area a couple times a day. Also, warm saltwater rinses.”
“I’ve never had a cavity and my dentist is amazed by this because I’ve had multiple root canals and crowns but that not because of decay…it’s from the tooth enamel breaking down from lack of nutrients and use of steroids over long periods of time.”
“Ice like crazy after a root canal. I’ve had three root canals with two failing and losing the teeth thanks to my Crohn’s. Putting a soft ice pack on my face post procedure was my lifesaver!”
“I’ve always been labeled “incredibly difficult to numb”—to the point where the dentist didn’t believe me, and I was about to hit the ceiling in pain when they started drilling. I never put two and two together that it could be related to IBD and none of my dentists have either.”
“I saw your post about your tooth. I would suggest following Dr. Michelle Jorgensen. She’s a functional dentist and talks a lot about gut health and dental health. She’s been on a few different podcasts talking about it as well. She also has a tooth powder that I use and love! For tooth pain, clove oil works great. Along with CBD oil—Met Naturals is my favorite. Turmeric oil is my go-to for pain. Arnica is also a natural pain reliever.”
“I have UC and have been incredibly nervous about my dental health since my diagnosis. I asked my dentist office about more frequent cleanings and found my insurance will cover four cleanings a year. So, now I go every three months. I know it can’t prevent everything, but I’m thankful for this bit of help.”
Some points to consider:
Shared Risk Factors: Some studies have found shared risk factors between periodontal (gum) disease and IBD. Smoking, genetic predisposition, and immune system dysregulation may contribute to both conditions.
Oral Health and Inflammation: Poor oral health, especially chronic gum disease, can lead to inflammation in the body. Inflammation is a common feature of both dental issues and IBD. The body’s response to oral bacteria in the gums may contribute to a systemic inflammatory response.

Microbiome Connection: Both the oral cavity and the gastrointestinal tract harbor complex microbial communities. Imbalances in the oral or gut microbiome may play a role in the development or exacerbation of inflammatory conditions.
Immune System Interactions: The immune system plays a crucial role in both maintaining oral health and regulating inflammation in the gut. Dysfunction in the immune system could contribute to the development or progression of both dental issues and IBD.
What you can do
Maintaining good oral hygiene practices, such as regular dental check-ups, proper brushing, and flossing, and addressing any dental issues promptly, is recommended for overall health, regardless of any potential association with specific medical conditions like IBD. If you have concerns about the relationship between your dental health and IBD, consult both your dentist and gastroenterologist for personalized advice based on your specific health situation. Some people in the IBD community reached out to me and said they get dental cleanings every three months and feel that’s a huge help in maintaining their dental health.
If you have IBD and need a dental procedure:
- Communicate openly with both your dentist and gastroenterologist about your medical history, including medications and symptoms.
- Follow a consistent oral hygiene routine to minimize the risk of dental issues.
- Discuss any concerns or questions you have with your healthcare providers.
Because we often have chronic inflammation in our bodies due to IBD, this could potentially affect the body’s ability to heal after dental procedures, including root canals. For those with IBD, there may be an increased sensitivity to infections or challenges in managing inflammation, especially as we try and limit NSAIDS. Prior to a procedure, make sure your dentist or endodontist is aware of all medications you take to make sure there will not be any oral health implications or interactions with your dental treatments.
Final Thoughts
Keeping up with all our medical care, including dental, can feel like a part-time and sometimes even a full-time job. Getting teeth cleaned twice a year and taking care of oral problems may get pushed down the list of priorities, but oral health is not something to be ignored. Poor oral health is often a reflection of a person’s overall health and can even be the cause of systemic disease.
It’s important to note that correlation does not imply causation, and several factors may contribute to the relationship between dental health and IBD. Additionally, individual experiences vary, and not everyone with IBD will necessarily have poor dental health or vice versa. While there is some research suggesting a potential association, the evidence is not conclusive, and more studies are needed to establish a clear link between dental health and IBD.