Traveling with inflammatory bowel disease (IBD) is rarely as simple as packing a suitcase and showing up. It’s logistics, emotions, planning, and flexibility. It takes a bit of hypervigilance. This layered on top of a disease that doesn’t take vacation days. But it is possible. And for many of us, it becomes one of the most empowering reminders that life with IBD can still be adventurous, and rich with new experiences.
This week on Lights, Camera, Crohn’s you’ll hear from two incredible IBD advocates, Kelly Dwyer and Rachel Verbanac. They both open up about their diagnoses, their anxieties, their coping strategies, and their go-to travel essentials. Their honesty and wisdom offer a roadmap for anyone who wants to explore the world without letting IBD call all the shots.


Meet Kelly: 21 Years of Symptoms, 7 Years Diagnosed
Kelly may have been diagnosed with Crohn’s disease in 2018, but she’d been living with severe perianal fistulizing ileal Crohn’s since the early 2000s.
“Before diagnosis, I avoided significant travel whenever possible because I was so ill. And when I did travel, I tried so hard to plan for every single scenario that it became stressful for me and everyone around me.”

Now in deep remission thanks to medication, Kelly still plans intentionally, but the difference is that the planning empowers her instead of holding her back.
She structures trips around:
- Her injection schedule
- The time of day she flies or drives
- What foods she eats before travel
- How to pace her energy
- And what she needs to stay healthy while surrounded by crowds
“I wear a mask, use sanitizer constantly, wash my hands as much as I can… it all helps me feel like I’m doing what I can to set myself up for success.”
Kelly on Travel Anxiety: The Trauma Stays with You
Despite years of remission, Kelly still carries fear rooted in lived experience.
“I constantly worry about not making it to a bathroom. Even though it has not happened in years, that trauma stays with you.”
Kelly also experiences nausea, anxiety and a whole lot of gas and burbling guts when she travels.

“Finding the right medication cocktail that keeps things calm and in order in my guts (and brain!) took a lot of trial and error, but was worth it for me to find a combination to give me confidence that I’ll feel like I’ve done everything I can to get the trip off on the right foot. I would recommend you ask your doctor or GI about Zofran, anti-anxiety medications in small doses, Gas-x, antacids, and other OTC medications that might help you to make sure they’re safe for you to take.”
She’s built a system that helps her feel confident when she’s traveling:
- A “Can’t Wait” restroom access card
- Depends or heavy-duty panty liners on days she’s unsure
- Change of clothes and wipes in her purse, not her carry-on
- Imodium and emergency meds ready to go
- Small meals before and during travel days
- Medication for nausea, anxiety, gas, and gut discomfort
“I had to learn to relax into the chaos of travel and not panic when plans change. Travel is unpredictable—but so is Crohn’s.”
The Power of Protection: Insurance (Both Emotional and Literal)
Kelly is adamant that travel insurance is non-negotiable.
“I have used travel insurance many times for flare-related cancellations. It can be heartbreaking to miss something important, but it’s not your fault. This is your reality, and you’re doing your best.”
She also communicates openly with travel companions, so expectations are clear and compassionate from the start.
“Find as much peace as possible. Asking for everyone’s understanding and compassion, is so important. I remind myself that it’s not my fault that I am unwell. It’s not anything I did to cause the flare. This is simply my reality, and I am trying my very best, even if it doesn’t always work out the way I’d hoped.”
Kelly’s Must-Have Travel Kit
Here’s what she never leaves home without:
- Bundaberg Ginger Beer
- Gin Gin’s Chews
- Alcohol wipes (to hijack the nausea signals in the brain!)
- Overnight pads
- A&D Ointment (for diaper rash and skin irritation from fistulas)
- Finger cots for applying ointment
- Small travel organizer for all my supplies
- Pill organizer
- Travel bathroom wipes
- N95 masks
- Travel sanitizing wipes
- Refrigerated Injection Canister
- On the go Applesauce to calm my upset stomach
- Travel rice cooker (when I need to cook gentle food in a flare)
- Heating pad
- Portable bidet
Kelly’s biggest piece of advice?
“Treat yourself with compassion, always. Build in extra time everywhere. Your comfort is worth it. Having a few extra hours at the airport to sit and read a magazine is much preferable to rushing through security lines and not being able to use the bathroom before getting on the plane because you’re late.”
Meet Rachel: A Travel-Lover Who Refused to Stop Exploring
Rachel was diagnosed with Crohn’s disease in 2021, right as she was going back to nursing school. Before that, she spent months living a nomadic lifestyle in New Zealand and expected to spend her twenties exploring the world. Her diagnosis meant rethinking what travel could look like. Requiring infusions changed everything.

“Hiking the Appalachian Trail used to be a dream, but with the need for insurance, pharmacy authorizations, infusion clinics, and access to university health systems… that lifestyle just wasn’t realistic anymore.”
But Rachel didn’t stop traveling. She adapted.
How Rachel Travels Now
Rachel describes herself as someone who “packs her anxieties,” but in a productive way.
Her prep includes:
- Bringing a med kit stocked with small doses of essential meds
- Monitoring hydration closely on travel days
- Planning meals and bowel habits ahead of time
- Understanding bathroom access in each country
- Carrying small local currency bills for paid restrooms
- Bringing a letter from her provider outlining her diagnosis and meds
“After many international trips, I’ve proven to myself that how I feel at home reflects how I feel on the road.”
Rachel also buys comprehensive travel insurance that covers pre-existing conditions, often from TinLeg, and encourages others to read the fine print carefully, especially regarding upfront payment rules.

“I feel much more secure knowing all medical bills will be paid for should I need anything abroad. Beyond health insurance, I have used the insurance for trip interruption and costs of delays. I also have my provider write me a letter stating my disease, common side effects, and my current medications. This letter can be useful when seeking care at a new clinic or if TSA should ever give you a difficult time (I have never experienced this). I like having the physical letter in the med kit.”
Bathroom Access: A Cultural Learning Curve
When traveling with others, Rachel gives them a heads up that access to bathrooms is a priority for her. Especially when traveling in Europe.
“Europe often requires a purchase to use a restroom. You cannot just run into a McDonald’s.”
Her strategy?
- Plan ahead
- Carry cash: Having a few small bills in the local currency is helpful to make a quick sale or pay at public bathroom stations in some countries.
- Use a bathroom every time you see one
- Keep the Crohn’s & Colitis Foundation’s “We Can’t Wait” card on hand
And she always tried to keep everything in perspective, even when the unexpected happens.
“Accidents are embarrassing, but you will most likely never see these people again. It is okay. You are okay.”

Travel Anxiety: You’re Not Alone
Rachel acknowledges the fears that come with IBD, but her message is clear:
Do not let IBD keep you from seeing the world.
Start small and your confidence will grow.
She now travels to Mexico annually and cannot imagine winters without it.
Nurse-Approved Safety Tips from Rachel
Some of her favorite reminders:
- Even healthy travelers get GI bugs—be cautious with food and water. Taking general precautions like only drinking bottled water in areas where the water might not be safe to drink, sanitizing your hands often, and avoiding touching your eyes and mouth are still the best ways to prevent infections.
- Avoid buffet sushi
- Choose made-to-order stations
- Read resort and food reviews. She checks out Google reviews, TripAdvisor, and Hotels.com to see what people have to say before she books a trip.
- Wear an N95 on flights to avoid illness and see if your travel companions will do the same to help keep germs at bay.
- Advocate for yourself with travel companions
- Read Google reviews quickly if you’re unsure of a restaurant, locals and travelers will share if they got sick eating there. Look for highly frequented places.
As a nurse, Rachel has these words of wisdom for our community, “Don’t let IBD keep you from seeing places and experiencing new cultures. Often as patients we have anxiety and unknown destinations can seem overwhelming and scary. Start small and your confidence will grow, promise.”
Rachel’s Travel Med Kit
She carries:
- Doctor’s letter
- Hand sanitizer
- Tylenol
- Imodium
- Pepto
- Tums
- Fiber
- Gas-X
- Benadryl
- Dramamine (also helpful for intense nausea)
- Zofran
- Liquid I.V.
- Band-Aids that are a few sizes
- Contact solution or small vial of artificial tears (I wear contact lenses)
- A few doses of Dayquil and Zyrtec—when changing the container medication comes in, be sure to write the dose (mg or ml or the number of pills) and how often you take it.
- A tube of triple antibiotic ointment and hydrocortisone ointment (for scrapes and bug bites)

Final Thoughts: You Deserve to Experience the World
Traveling with IBD takes more planning, more flexibility, and more courage than most people will ever understand. But as Kelly and Rachel show, it’s possible and it can even become empowering.
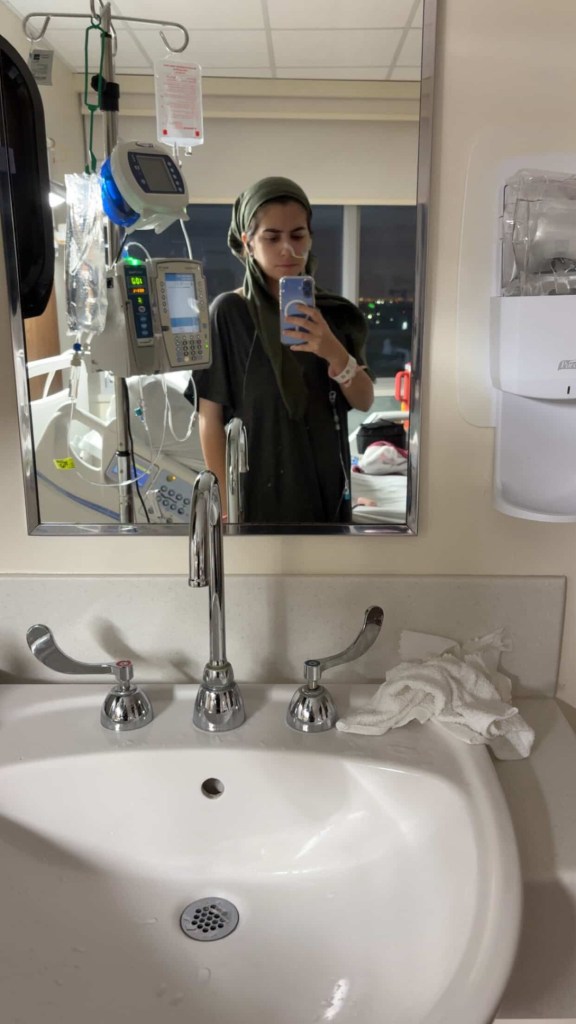
As someone who was diagnosed with Crohn’s more than 20 years ago traveling can still make me feel a bit uneasy. I always keep pain medication, Zofran, and Dramamine in my carry on. If you have to pack your biologic medication, keep that on you as well. It’s important to check how long your injection can be out of the fridge. Nowadays, Humira for example, can be unrefrigerated for up to 14 days. If you have to do your injection while away from home, make sure to have alcohol swabs and an ice pack (if you are used to using one).

I never drink caffeine prior to flights or long road trips, and I eat very light until I am at my destination. I try to dress as comfortably as possible, and do not restrict my belly in any way. The moment I get to my hotel room I take off my travel clothes and shower. If you are traveling and feeling symptomatic, it can be helpful to alert your care team at home and also do research beforehand about local hospitals so you have a game plan in place should you be facing an acute flare that may require a trip to the emergency room.
Whether you are taking a weekend road trip or boarding a long-haul flight, remember:
You’re allowed to take up space.
You’re allowed to prioritize your needs.
You’re allowed to choose comfort over speed.
You’re allowed to protect your energy.
And most importantly:
You deserve to make memories that reach far beyond the walls of your disease.
Additional resources
Traveling with IBD | Crohn’s & Colitis Foundation
Crohn’s Disease: Plan Ahead to Make Travel Easier
Travel Tips When You Have Ulcerative Colitis
Tips for Long Travel Days When You Have Crohn’s Disease