Whether you’ve experienced one colonoscopy or 20, you know the process is far from enjoyable. This past week while scrolling through Instagram I came across a story an IBD caregiver posted as her young daughter prepped for her scope. During the video she explained how her husband rolls dice, and whatever number it lands on is how many sips their daughter has to take of prep. I was amazed at this brilliant trick to ease the struggle of getting the prep down, and it inspired me to dig a little deeper and ask the IBD community what their “tips and tricks” are.
This week on Lights, Camera, Crohn’s read firsthand advice from caregivers and patients of all ages. My hope is that you find comfort and maybe even a new idea or two to make your next prep a little less stressful.
Firsthand advice for pediatric IBD caregivers
Mara’s daughter has IBD and has already been through eight colonoscopies in just five years. She says the dice game was a huge success for their family the first time around:
“She was at the perfect age for a little competition as motivation with a reward at the end for the winner…of course she always won. It was honestly so easy to prep her I was shocked.”
However, being NPO (derived from the Latin saying ‘nil per os’ or nothing by mouth/no food or drink) after midnight was NOT easy.
“There were lots of tears and anger directed at us. We bought her a special blanket and stuffed animal, which helped diffuse some of that anger.”
As many caregivers know, every prep is different. Mara recalls their second scope being much more difficult, requiring hospitalization and an NG tube after her daughter couldn’t keep the prep down. Now, they focus on giving their daughter as much autonomy as possible, letting her choose flavors, snacks, and activities.
“On prep days or days, she must be NPO, dad and I also follow that diet. It gives her a sense of belonging and that we are struggling right alongside her. We’ve done it for all eight scopes, and we will continue to do it if she needs us to.”
Over time, Mara says they let their daughter lead as much as they can. They give her a “yes” day.
“Whatever she wants (within reason) to eat or drink. Gummy bears, sure. Popsicles, sure. Want to try to mix three different Gatorades? Why not? She wants to watch TV while she preps or play hockey, absolutely.”
Emily’s Family
Emily has three daughters with IBD (now ages 9, 12, and 15) who’ve been doing preps for over a decade. Their youngest had to prep for a scope when she was only 21 months old. Their top tips include:

- Only prepare 8oz of the drinking mixture at a time. With MiraLAX prep, we let them pick a new flavor to mix each 8oz.
- Think outside the box with the liquids for MiraLAX! One preferred water once! (With other electrolyte drinks that day.) One daughter does her whole prep with tea and chicken broth. (Add MiraLAX after the liquid is warmed.)
- Use distraction!! This is our biggest piece of advice. We surprise the girls with a new activity the day of prep. They know there will be something fun to do – just not what it is. We have gotten Lego sets, multi-step craft projects, etc. We pick something that we can partition up and give them one part at a time in celebration for ounces drunk!
- Keep them active. We have found that the girls tolerate the large amounts of liquids better if they get up and get moving! In the warmer months, they go walk laps around the driveway between cups of the prep.
- Pick the “fun” liquids together ahead of prep day. Since they normally cannot have juice or soda, they pick out a few drinks that they are excited to have. This helps them to drink more, once the MiraLAX prep is complete.
- I set timers for myself for the day of prep for every 10 mins or so. Just to check in on their drinking. It’s easy to lose track of time and accidentally go 30 mins (or more!) without drinking.
- Pack a bag of supplies for the scope day. We always take extra clothes and baby wipes for any accidents. Games/books/crafts are great to keep the girls distracted during the wait before their procedure time. We take some water/light snacks for afterwards. (Check with your providers to see what/when your child can eat afterwards.) Chapstick is always requested by mine now too.
- Remember that you can speak up and (nicely!) ask for what your child needs to make them comfortable. For example, at our hospital, the kids usually get their IV’s after they are sedated with some gases through their breathing mask. This is great to avoid needle anxiety for many kids. However, mine have taken a dislike to the masks and the smell of the gas. Since they get regular med infusions, they prefer to get their IV’s back in the holding area and then use the IV for their sedation to sleep. While not the normal procedure, the anesthesiologists and nurses have kindly worked with us to do it the way my kids prefer.
Cindy’s Perspective
Cindy, mom to a teenage daughter with Crohn’s disease, says scheduling scopes early in the day is key. Even if you have a teen who likes to sleep in, sleeping in is worth nothing if you already feel like crud due to the prep. She emphasizes advocating during IV placement and following your gut as a caregiver:
“A parent’s intuition of how much is too much comes into play, and you’ve got to listen to that voice. Tell the nurse you (parent and child) did your best to complete as much of the prep as possible. If you can’t finish it to a T, they can still make it work. They know they are working with a child. If they are having trouble placing an IV, advocate for your kid. Give them two tries and then request another person to try. We’re still traumatized from watching them work for 10 minutes to get an IV into my dehydrated and scared 9-year-old, and I think that trauma will live with us both forever.”
She also believes in being honest with your child without over-preparing. Start the conversations when it’s time, but don’t talk about it for days or even hours beforehand.
“This is not going to be fun, and it won’t feel good. But I know you can do it and we are going to do it together because I will be beside you every step of the way. Here are the steps we will take and outline them in age-appropriate detail. Let’s think about how amazing this is going to be once it’s done! This is our focus for the next 24 hours… that moment when it’s done… that will be the best! As soon as you are done at XYZ time tomorrow, we can celebrate and go back to normal life, and you can eat whatever you want.”

Additional feedback for pediatric patients
“For pediatric prep, popsicles are necessary. Blue popsicles allow kids to “poop blue,” which many like. The Gatorade with the MiraLAX is the easiest for them to get down. We tried magnesium citrate once and it was a disaster. Gatorade is where it’s at. Also, we make it a party. Popsicle party. Jokes and TV while pooping. Anything to keep the mood light.”
“Turn the ordeal into a scavenger hunt by completing parts of the prep with small stickers to earn up to something whether it be completing a picture or something to distract when prep is working.”
“My daughter’s first prep at home didn’t go well, but prep while in-patient thru NG tube really worked.”
“If the hospital or your GI team has a Child Life specialist, they can send prep books to families ahead of time so they can help prepare kids for what to expect the day of the procedure.”
“Bribes! Lots of bribes! New toys or games. Legos keep little ones busy. Family doesn’t eat in front of them. Lots of snuggles. Clear your schedule to spend time with them. For young kids, put all food out of reach or lock the pantry so a hungry little one doesn’t get into something they can’t have and make you have to cancel the procedure, which is always my fear!”
“I have a prep approved Starbucks order—Mango Dragonfruit refresher, Venti, no ice, no Dragonfruit fruit inclusions, peach juice blend, in my personal cup … I like to line up cups so I can visually see how much is left and removing one feels like an accomplishment. A seasonal suggestion is using an advent calendar and dividing prep by 24 and opening one door after each one…just make sure the prizes are not food!”
“Arts and craft activities and projects can be a good distraction. Recently gave a sensory art bin to a VEO-IBD patient through their first scope as a kid it helped me to have new things to do.”
“My mom fasted with me when I was doing the prep as a kid! My tips now as a mom myself are to make Jello without Red 40. Ramen seasoning dissolved in water tasted way better than broth to me as a kid…I know that’s not good for you. I would make it a fun and relaxing day, so your kiddo is distracted. I would recommend not watching TV or YouTube because there are so many advertisements for food everywhere and it didn’t help distract me much. I advise having a movie marathon instead!”
“We didn’t eat out much when I was a kid, so eating out with my parents only was a big treat for me to look forward to after starving the day before! Back in the day, GIs used to do a combination of drinkable prep and suppositories for pediatric patients, and I’m glad my mom did the suppositories for me because it was not something else you had to drink. Ask pediatric GIs about low consumption prep so your child doesn’t throw up.”
“When I was a pediatric patient, my mom took me to the store to pick out different drinks for the mix, Jello flavors, etc.… which would make it fun picking it out myself and this also gave me a sense of control in a very out my control situation. My mom always fasted with me, which I appreciated not feeling alone in it. I was also able to pick the restaurant to go to after for something to look forward to!”
“Have your child drink their prep in a fun container., a Disney theme with a silly straw. For adults, use a wine glass or fun mug. Cheers!”
“My 12-year-old just had their first colonoscopy. As a Crohn’s patient myself, I have done one every other year for 25 years and it was hard to watch him go through it. He was tougher than me. The hardest part was him not eating! He had to do a full two days of clears only—per our doctor’s recommendation. That’s my hack as an adult, too. I start taking a Dulcolax dose and not eating a day or two earlier than recommended. You only have to drink the drink until it’s clear in the toilet. The milder/longer prep is easier on me and saves me drinking half the magnesium citrate drink.”
“My daughter couldn’t get any of the prep down at age 16 and by this summer, at age 19, she felt ready. This time we tried over the counter prep of MiraLAX and Dulcolax. The doctor said if she did it this way, she would need to fast for 48 hours instead of 24. She was fine with that. She started taking a couple of Dulcolax tablets at 5 pm the night before. Then, we put half a bottle of MiraLAX into Sprite. She drank a cup every 10 minutes until it was gone. We did the same thing a few hours later. She was clear before going to bed at night. It was easy and stress-free for her.”
“My parents would set me up with my iPad for movies, a desk chair, and a blanket in the bathroom so I could go back and forth from the toilet easier.”
“Make MiraLAX with white grape juice instead of Gatorade! Drink with a fun straw so you can put it on the back of your tongue and taste less. Put on headphones with loud music to distract your sense from the taste so you can drink the prep faster.”
“I confirmed with my child’s GI that colorless cotton candy is a clear liquid! Obviously in moderation, but this could be super helpful for kids and adults who need a different texture than liquid or gelatin.”
Prep Hacks for Adult Patients
Our IBD family had plenty of creative hacks for adults, too:
“The MiraLAX + Dulcolax prep hands down!! I’ve tried them all, and it’s tasteless and easiest.”
“Lemonheads or lemon jolly ranchers RIGHT after you get done drinking a dose!”
“Gummy bears and lifesavers! I love having stuff to chew. I also had pickle juice shooters, which gave me some salty/sour taste to balance all the sweet stuff. I also keep my schedule open for the remainder of the day and allow myself to relax.”
“I put my Suprep in the fridge (even though it says not to) and it makes it SUBSTANTIALLY easier to drink (and doesn’t seem to make it less effective in any way). I also buy myself a new book to read or save a special TV show episode, so I have something to look forward to when I’m drinking prep at 2 in the morning. Colonoscopies are miserable and until they figure out how to make them a nicer experience, it’s great to team together to gather the best tips.”
“Clear Gummy Bears!! This keeps it fun for all ages! Here’s a recipe!
“Drinking chicken broth throughout the day. This gives energy and takes away the bad taste of the prep drink. As a kid, my sister used to make a colonoscopy prep kit. Every 8 oz. I drank; there would be a little gift or activity to do. For example, after the first 8 oz., I got a nice bottle to drink the rest from. The next thing was a Lego kit or a paint by number.”
“I begin my prep four hours ahead of their suggested time, so I can sleep through the entire night. Getting up in the middle of the night, especially for children to complete round two of the prep is just borderline inhumane. What a nightmare. The catch is waking up and hydrating with enough water before the anesthesia cut-off which requires not to drink anything 2 hours before the procedure.”
“Wet wipes and diaper cream are super helpful!”
“A lot more MiraLAX than the prescription prep. And gummy bears (except red ones) are a gamechanger. They let you feel like you’re eating, but they liquify in your gut.”
“Rotate flavors and get some protein through broths. Have broth, then 2 hours later do Jello or change the texture and taste, then 2 hours later do broth and rotate.”
“Strain chicken noodle soup to just have the clear broth, it has more sodium.”
“Avoid eating vegetables/fruits/seeds three days before. Taking preps that you can take with a glass of water and then drink two liters of tea or water.”
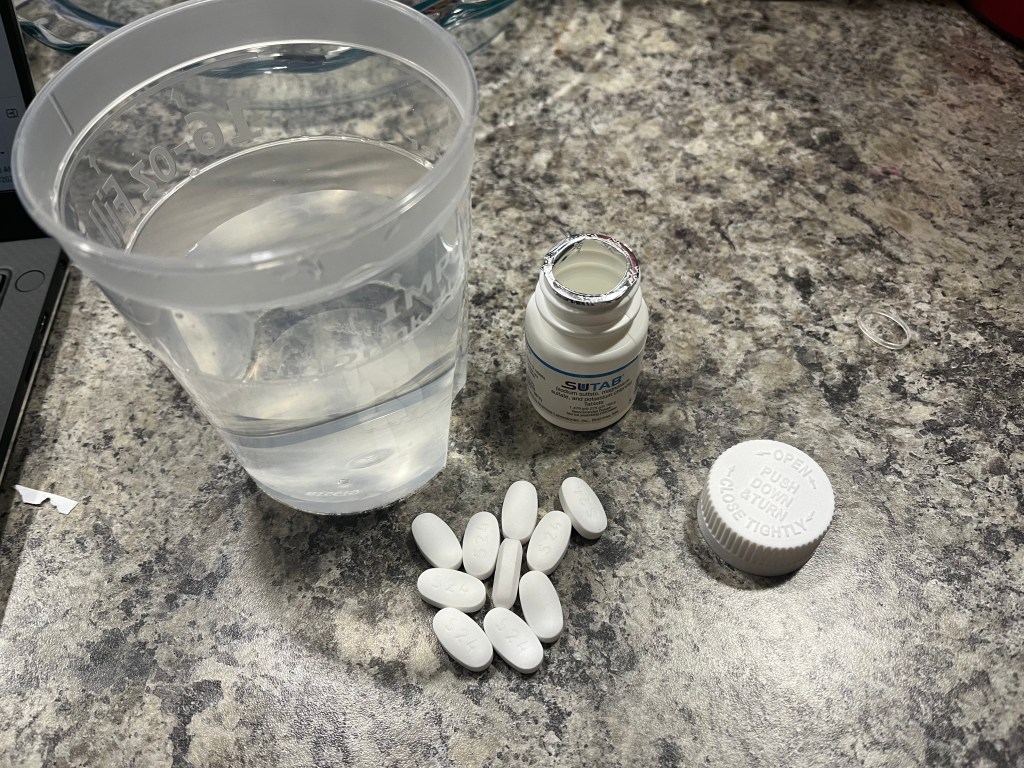
“My son, Andrew, has autism and Crohn’s disease. When he has to do colonoscopy prep, he likes to listen to Disney music and use a timer. Andrew is almost 30 years old and has been having to do colonoscopies since he was 17. This past year, for the first time, he did the pill prep and loved it. He used a timer to tell him when to take the next pill. Andrew told me he will never go back to liquid prep. Pill prep was so much easier for him, especially with his sensory issues.”
“Take notes on all preps you’ve been assigned and take notes and photos of what it felt like. I found one that was less painful for me, and I always request it. I also alternate sips out of a straw with apple juice. I drink the prep in my kitchen, near a bathroom, and watch TikTok’s while drinking to distract myself.”
“I only eat soft foods 2-3 days before, make sure to hydrate, and follow the instructions they give about not eating things like seeds or nuts a week before.”
“Have a bidet and diaper cream ready.”
“Desitin, Gatorade that is the Frost Glacier Cherry flavor (not red) frozen or really cold to help me stay hydrated.”
“Make freezer pops out of the Gatorade prep mix.”
“For me—finding fun drinks, whether a tea at Starbucks or stocking up at the grocery store, really makes it feel less horrible. I started this as a teenager. I make a list of movies or shows I want to binge. If you’re comfortable with it, have a friend there to distract you—at 15 years old, my boyfriend stayed with me all day for my surgery prep which was the same as a colonoscopy and we watched movies and he distracted me/made me laugh and at times I forgot what was going on!.”
“Savory liquids to balance out the sweet!”
“Mix the prep with Crystal Light Lemonade—instead of the lemon mix the pharmacy provides. Drink the prep through a straw and suck on hard candy (e.g., Werther’s Originals) in between doses to get rid of the taste and have something to look forward to.”
“Take SUTAB (pill prep) and Zofran and then fall asleep. Your bowels will wake you up and you’ll avoid the nausea but start the pooping process. I do the same for the morning dose! If you vomit, at this point it’s fine, just hopefully after the nap and pills are digested!”
“Gummy bears/worms!”
“Pill prep has been a gamechanger for me!”
“Extending the clear liquid diet an extra half day or full day helps a ton with prep.”
“You have to have a movie downloaded on a device that you can have in the bathroom and a pillow for the toilet seat for your back. I’m a fan of disposable diapers because after the first several poopy poops, you get to the drizzle stage and then it’s annoying to have to get up every two seconds towards the end. They also come in handy when you’re sleeping and when you’re traveling to the procedure.
“Before I have a colonoscopy I write down positive affirmations and thoughts and there is like a Table of Contents that’s like “When you’re sad” or “When you need a good laugh” and it really helps me though the ups and downs, although it may sound silly. I choose what to drink and I always have my good luck drink which is blue Gatorade.”
“Use nuun electrolyte drink instead of Gatorade!”
“My personal hacks are to follow what you know works for you. I followed the timings of when to take what from the last instructions and it wasn’t the cleanest prep. I should have listened to my gut and started doing that earlier. I resort to drinking Ensure Plus instead of just relying on broth and soft foods to keep me feeling full. It’s helped me SO much. I know not everyone can tolerate it or like it, but when I was on a liquid diet about a year ago for two months, I only had Ensure Plus. I got used to it. It’s now a lifesaver, especially if I’m traveling or on the road and not sure what food I will have access to. It helps to start the diet a bit earlier, so mash and fish instead of just toast and pasta.”
“I mix apple juice with my Suprep! I also always buy bone broth or stock because the protein per cup is higher. I like the Zoup brand because there’s 3 or 4 gram of protein per cup. I also get the College Inn brand bone broth which has up to 10 grams of protein per cup.”
“Gummy bears!! Just not the red or purple ones. Just being able to chew something helps! Progresso Chicken Soup. Use a metal strainer to strain out all the solids and then sip the broth. It’s thicker and has more flavor than regular stock and it’s just more satisfying.”
“Remind yourself “this is only temporary.” Having loved ones supporting also helps to distract a little, which makes it easier to get through. Focusing solely on drinking cup after cup can seem very overwhelming.”
“Start a low residue diet a few days early even before your doc says to. Mix prep with Sprite. Have hard candies or gum to chew on while doing prep. Use a measuring cup or something to lines to indicate how much to drink.”
“I really love the Trader Joes less sugar lemonade mix with water for my prep. I chugged and it was so delicious! Also, ice pops like the good pop brand were yummy.”
“Gummy bears! Making ice cubes out of juice and chewing on the ice.”
“Make sure it’s cold! Drink with a straw, chew Juicy Fruit gym in between drinks, this helps cut the saltiness. Do two-step prep if your practitioner allows it (half the night before and the other half in the morning). Ask if you can use one of the lower volume prep or the MiraLAX and Gatorade prep.”
“For the MiraLAX prep I use two different flavors so I can alternate when I get sick of one.”
“Mix the prep early and put it in the fridge. Have music and TV on to help distract yourself.”
“While most people say to drink it cold, I prefer my prep at room temperature so I can chug it faster.”
“Always lots of ice and drinking thru a straw. Big gulps. Have a station in the bathroom with a laptop streaming Netflix. I also got a Bidet before my last one!”
“Gummy bears! I buy the Haribo ones and don’t eat the red ones. My favorite prep hack thus far. It’s great getting to chew something when everything else is liquid.”
“Lots of mint tea when the cold chills kick in a few hours before you have to go in for the procedure.”
“Use a Pedialyte jug and ensure it is very cold and drink the prep with a straw. The slower you drink, the worse it is. I always chug it super-fast through a straw and it gives me 10-15 minutes between each cup. Have lots of other drinks that you don’t normally consume to make it fun and have lots of juice, Jello, soda, and popsicles on hand!”
“I’ve turned prep days into self-care days. I binge shows, nap, relax, and try to take care of myself.”
“I like to alternate between sweet/cold beverages and salty/warm soups when I am trying to stay hydrated before starting prep. Sprite/popsicles/lemon ice and then chicken broth.”
“I chase my prep by sucking on approved colored Lifesavers. They truly are a lifesaver for me. I could never do it without them.”
“I recommend the pill prep instead of liquid prep if you’re neurodivergent or have issues with taste and textures. Maybe keep a backup on MiraLAX and Gatorade or juice in case you can’t tolerate the liquid prep. If you know you get nauseated, take prescription anti-nausea medication like Zofran before you begin the prep. I like Squatty Potty and having wipes to dab and pat my skin. A Peri Bottle can be useful. If you’re prone to hemorrhoids or know you have vascular issues like pelvic congestion syndrome, apply hemorrhoid cream in advance. Keep Zinc Oxide handy if it starts to burn or feel raw. Get into comfortable clothes that’s easy to get in and out of in the bathroom. I personally use a heating pad and Bentyl for intestine cramping. I usually make sure I’m scheduled first thing in the morning, and I ask for extra IV fluids.”
The Takeaway
Colonoscopy prep is a universal challenge in the IBD community, whether you’re a child facing your first scope or an adult whose been through dozens. But as the stories above reveal, there are countless ways to make it less daunting through creativity, distraction, teamwork, and sometimes sheer humor.
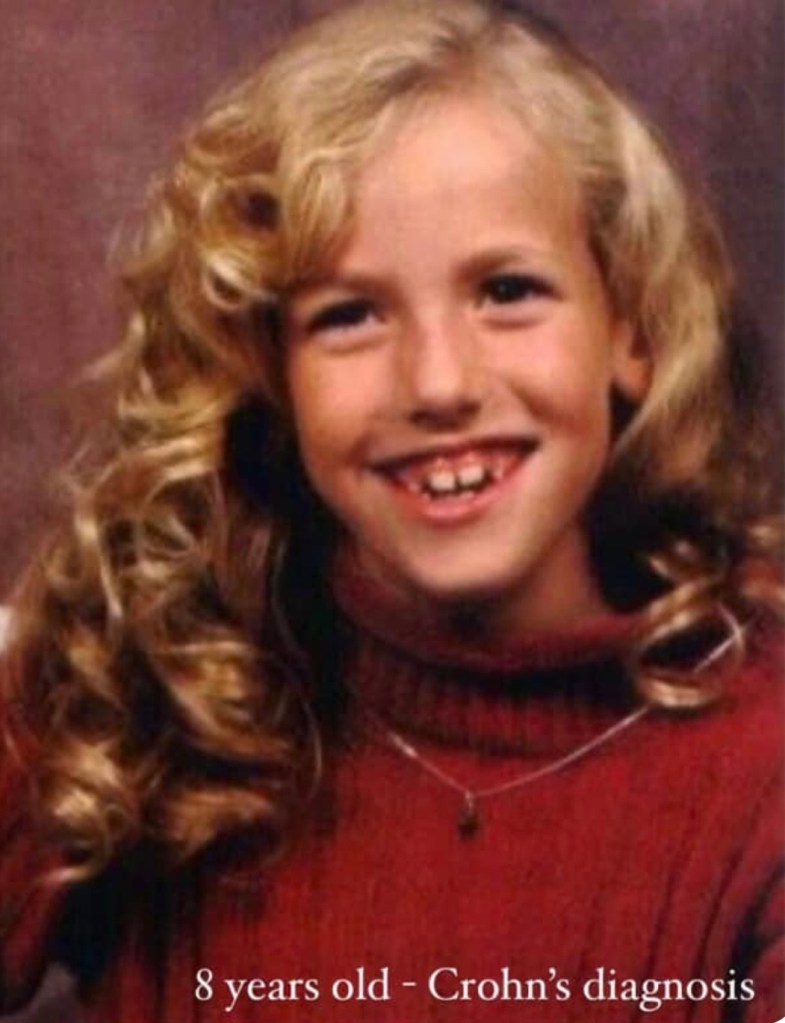
I personally start a full liquid diet 4-5 days before my scope to ease the actual prep. I make sure I have Zofran on hand to manage my nausea (I always vomit, regardless), and I prefer the SUTAB pill prep. I’ve done multiple preps since being diagnosed with Crohn’s disease in 2005, and my last three preps, SUTAB pills have been the “most tolerable.” While MiraLAX/Dulcolax is popular, I never enjoyed having to drink such a large volume of liquid. Having gummy bears on hand is also a necessity for me! My husband always takes the day off work, and we go out to breakfast and spend the day together afterwards as a reward for all I went through.

If you’re gearing up for a prep, remember you’re not alone. Thousands of IBD patients and caregivers are walking this same path and learning tricks along the way. Find what works for you (or your child), advocate for needs, and give yourself grace. And once it’s done? Celebrate that victory meal and the relief of getting through another milestone in your IBD journey.