Getting a colonoscopy when you have Inflammatory Bowel Disease (IBD) carries a distinct set of challenges and trauma compared to the average person receiving a colon cancer screening scope. I underwent my 10th colonoscopy this past week as part of my Crohn’s disease surveillance and heard the word “trauma” on multiple occasions.
I received the following public comment on an Instagram post following my colonoscopy, “You seem to have trauma around colonoscopy prep. I get it, but I don’t. Childbirth is traumatic but colonoscopy prep is not. It sucks, but really not traumatic. The flu sucks, strep throat sucks, why is this so hard for people?”
…to which I responded, “Do you have IBD?”…radio silence.
*Side note—none of my 3 child births were even close to traumatic, they were all joyous, uneventful, and happy occasions. But I digress.*

I had a wonderful nurse get me ready for my scope and give my IV, I let her know I have terrible veins and that I’m a tough stick. Once the IV was started she said that it appeared I have trauma around IVs…which I said was correct. While I appreciated her recognizing this it also felt a little bit judgy. During a prior hospitalization it took EIGHT tries to get an IV started. These difficult medical experiences cause trauma. It should not come as a surprise to anyone dealing with an IBD patient that what may seem run of the mill to an average person is not the same for us. I have to tell myself not to roll my eyes when a 70-year-old tells me how “easy” and uncomplicated their colonoscopy was. Happy for them…but their experience is much different than mine.
My most recent colonoscopy experience inspired me to dig a bit deeper and help to articulate why it’s hurtful and not helpful when you try and compare a “healthy” person’s experience getting a scope compared to someone diagnosed with IBD.

Oftentimes we receive confirmation of our IBD diagnosis after a colonoscopy. The results of a colonoscopy can significantly impact treatment plans, which may heighten stress. The fear of bad news—such as disease progression or the discovery of dysplasia—can weigh heavily. We not only have to rule out colon cancer (due to our elevated risk), we also have the weighted worry about hearing we could have active disease and inflammation going on. If that’s the case we may need to stop our current treatment, start a new treatment, need surgery, etc.
Unlike the average person who may not need a scope until age 45 and then not for another 7-10 years after, we know we may need to go through the ordeal multiple times a year, annually, or every other year starting whenever we’re diagnosed (as a child/in our 20s). The frequency of needing to go through prep and the procedure is astronomical compared to the typical person and when you’re way younger than 45 and have to go through a scope it builds resentment against your body, something our healthy peers and caregivers can’t truly grasp unless they’ve lived it. The cumulative stress of repeated procedures can lead to heightened anxiety and emotional exhaustion.

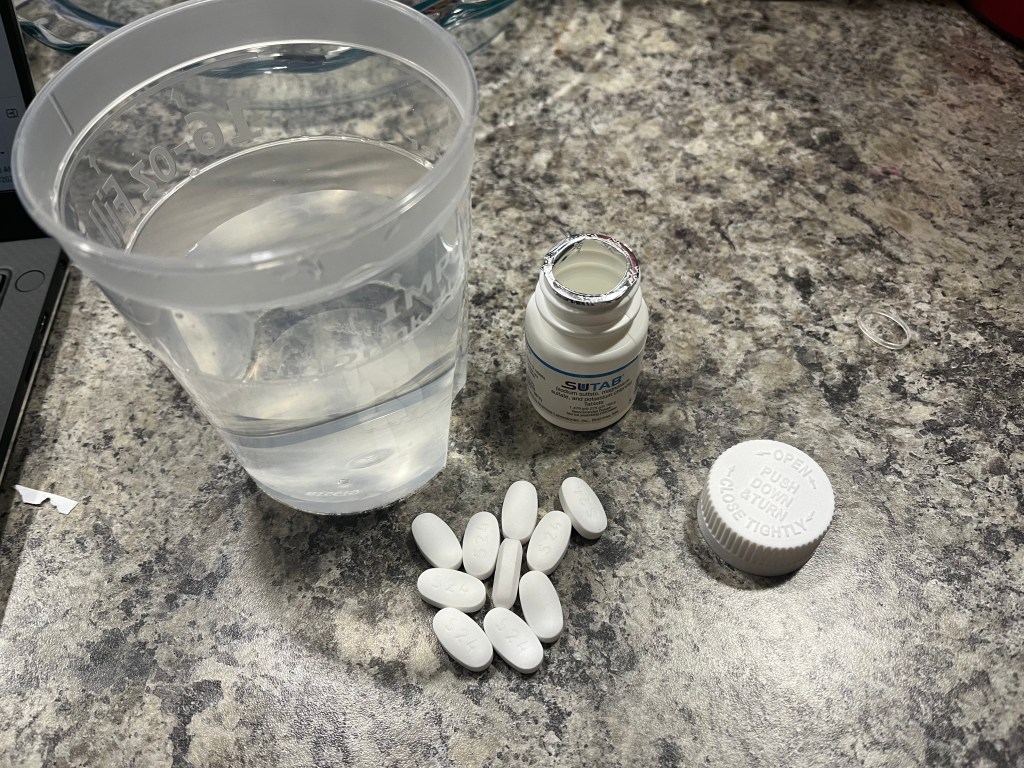
Our digestion is different from yours. Prep can induce abdominal pain, nausea, vomiting, and bloating that mirrors flare symptoms to us and this in and of itself can feel traumatic. People with IBD frequently experience inflamed, ulcerated, or narrowed sections of the gastrointestinal tract. During a colonoscopy, these areas may be more sensitive, leading to increased pain and discomfort compared to individuals without the condition. The bowel preparation process—which involves consuming large amounts of laxatives to clear the colon—can be especially grueling for those with IBD. It may exacerbate symptoms like diarrhea, cramping, and dehydration, making the days leading up to the procedure particularly difficult.

Many of us take the prep a step further and start a liquid diet days before the actual prep to try and “ease” the process. I personally put myself on a full liquid diet 4-5 days prior to my scopes and then a clear liquid the day before. This takes a great deal of willpower, especially as an IBD mom making school lunches and meals for my kids, while not being able to eat any of it. Caring for a family while running on fumes is not for the faint of heart. It’s a challenge to have the energy to function while feeling hangry. Understand that we might feel irritable, fatigued, or anxious during the preparation and recovery process. Provide a judgment-free space for us to express our feelings. I’m not one of those people who feels comfortable eating a light breakfast the day before a scope, because I fear not being cleaned out enough and having to go through the experience again sooner than I need or want to.

How to Be Supportive
- Acknowledge Their Experience: Validate their feelings and recognize that colonoscopies are more than a simple procedure for someone with IBD. Avoid dismissive comments like “It’s just routine.”
- Offer Practical Help:
- Assist with transportation to and from the procedure. Offer to babysit if the person has kids or needs help at home with childcare.
- Help prepare supplies for the bowel prep process, such as clear liquids, electrolyte solutions, and soft toilet paper.
- Offer to stay with them during recovery if needed.
- My husband always makes a point to take our kids out to dinner or try and not eat in front of me while I’m prepping, this makes a world of difference. We also always go out for a big breakfast or lunch date immediately following the procedure.
- Provide Distractions. During the prep period, suggest activities to keep their mind off the discomfort, such as watching movies, playing games, or listening to calming music.
- Encourage Communication with Healthcare Providers. If they’re particularly anxious or in pain, encourage them to discuss these concerns with their doctor. Sedation options or anti-anxiety medications might help make the procedure more tolerable. I always make sure I have Zofran on hand to take prior to my prep to help with nausea. I still always vomit at least once, but it does help.
- Respect Their Privacy: Everyone copes differently. Some people may want to talk about their experience and post about it on social media, while others may prefer to keep it private. Follow their lead and respect their boundaries.
Final thoughts
Colonoscopies are a critical tool in managing IBD and being proactive about colon cancer screening, but they can be uniquely challenging for those living with Crohn’s or ulcerative colitis. By understanding the physical and emotional toll of these procedures, friends and family can provide better support and help ease the burden.
My ask for friends, family members, and medical professionals with patients or loved ones who have IBD and are undergoing or gone through a colonoscopy is to refrain from comparing your own experience with us. Show compassion. Be kind. Remember that colonoscopies carry a sense of trauma for many of us, and for good reason. We are not weak. We are not complainers. If you lived our reality and been through what we have, I guarantee it wouldn’t feel like a walk in the park. Not many 41-year-olds I know have had 10 colonoscopies. With patience, empathy, and practical assistance, you can make a difficult experience a little more manageable for someone with IBD.









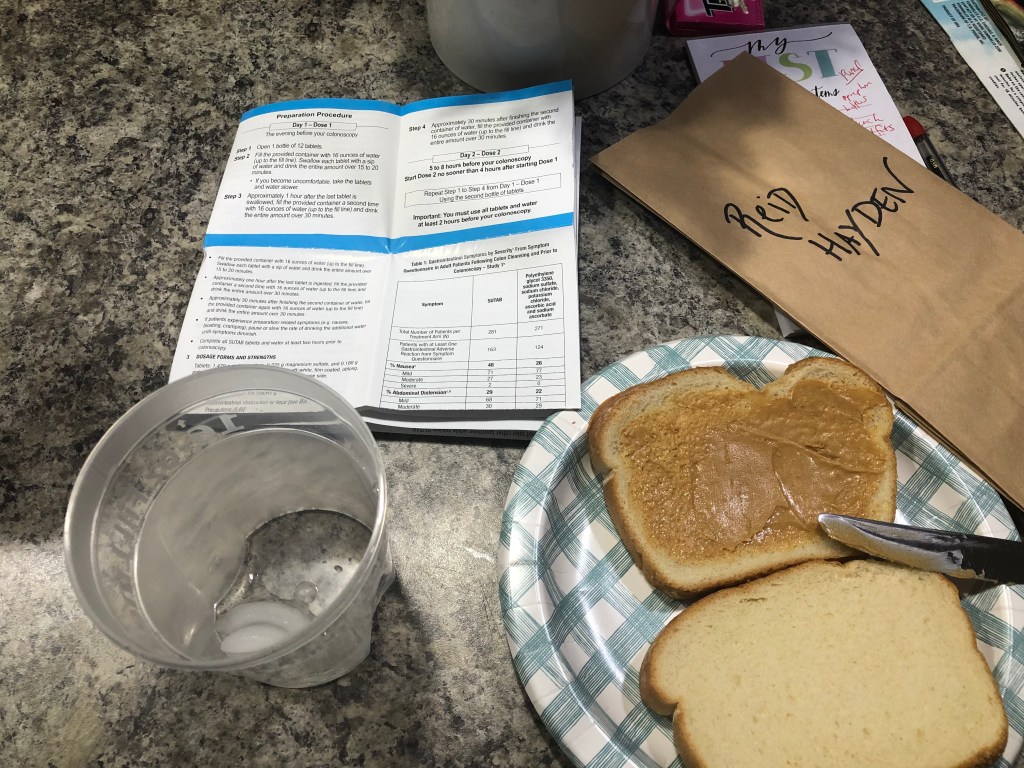







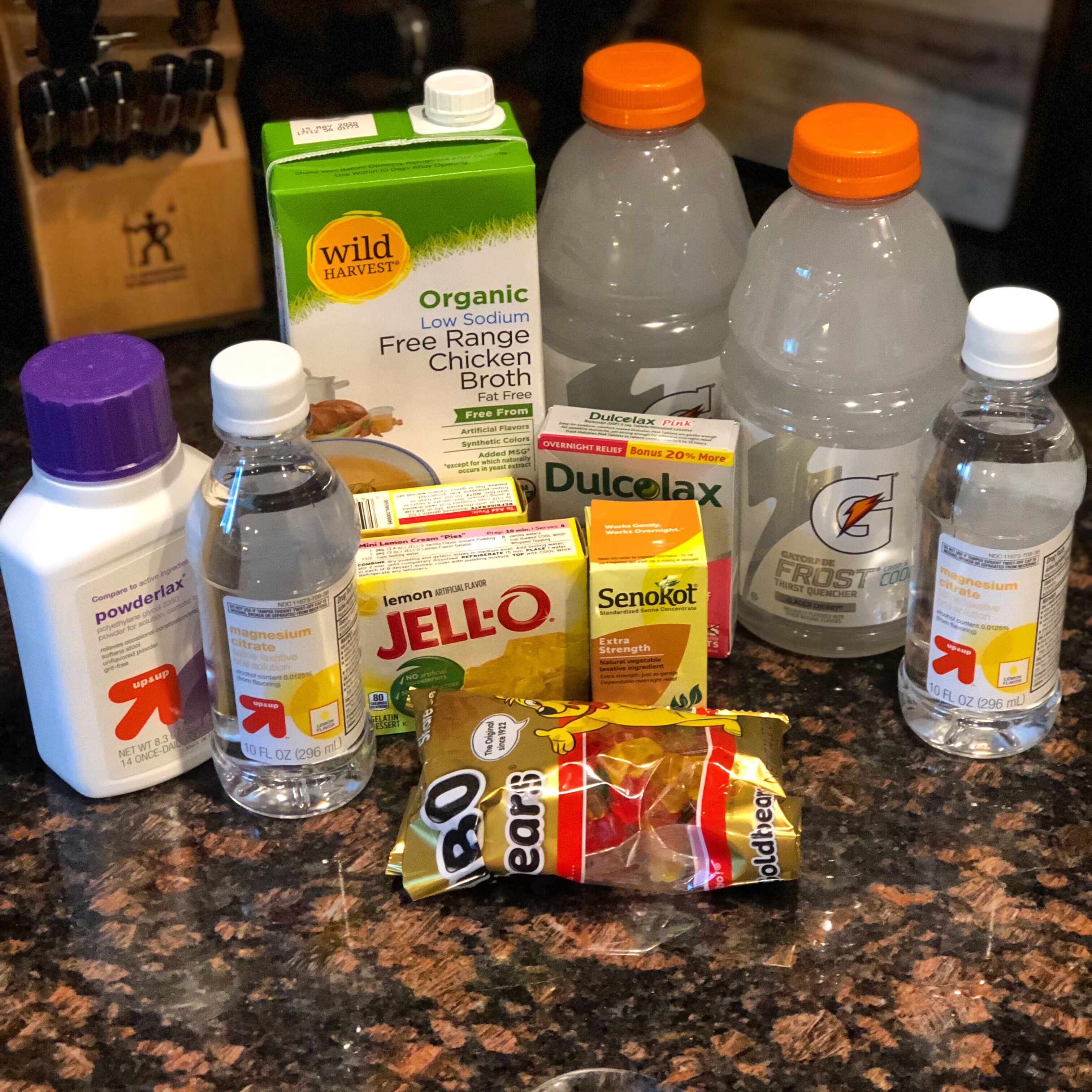
 Boys and girls, this is a game changer. Gummy bears are considered a clear liquid because they liquify upon digestion, much like Jello. In the days leading up, you can eat all the colors, but 24 hours before your scope stay away from any red, orange or purple as those colors are not allowed during prep. I used gummy bears to chase the magnesium citrate, two bears for every sip! It was also a nice treat and it felt good to actually chew something after only having liquids for days.
Boys and girls, this is a game changer. Gummy bears are considered a clear liquid because they liquify upon digestion, much like Jello. In the days leading up, you can eat all the colors, but 24 hours before your scope stay away from any red, orange or purple as those colors are not allowed during prep. I used gummy bears to chase the magnesium citrate, two bears for every sip! It was also a nice treat and it felt good to actually chew something after only having liquids for days. Look up menus and decide where you want to treat yo’self. Along with that first meal, I try and plan something fun to do. This time around my husband and I went shopping after breakfast and then we went out to dinner and to a light show at the Botanical Gardens (where we got engaged!). Knowing I had that to look forward to, helped me a great deal!
Look up menus and decide where you want to treat yo’self. Along with that first meal, I try and plan something fun to do. This time around my husband and I went shopping after breakfast and then we went out to dinner and to a light show at the Botanical Gardens (where we got engaged!). Knowing I had that to look forward to, helped me a great deal! My compassionate little 2-year-old even held my glass of prep with me and didn’t want to leave my side when I went to the bathroom. (lucky him!)
My compassionate little 2-year-old even held my glass of prep with me and didn’t want to leave my side when I went to the bathroom. (lucky him!) In the days leading up, my GI recommended I drink whole milk or chocolate milk to get some protein for the baby. (I chose not to do this because my stomach can be sensitive to dairy.) I made sure Sophia got a couple bottles of formula each day, since my breastmilk was probably lacking it’s normal nutrients.
In the days leading up, my GI recommended I drink whole milk or chocolate milk to get some protein for the baby. (I chose not to do this because my stomach can be sensitive to dairy.) I made sure Sophia got a couple bottles of formula each day, since my breastmilk was probably lacking it’s normal nutrients. It’s in these moments where I pause and reflect with positive internal self-talk. I think about family members and friends who inspire me. I pray to God for a smooth procedure and good results. I try and breathe and relax the best I can.
It’s in these moments where I pause and reflect with positive internal self-talk. I think about family members and friends who inspire me. I pray to God for a smooth procedure and good results. I try and breathe and relax the best I can. Rather than rely so heavily on achieving remission, focus more on how you feel each day. Are you having more “feel good” days than symptomatic days? Are you able to function and complete tasks personally and professionally without your health getting in the way?
Rather than rely so heavily on achieving remission, focus more on how you feel each day. Are you having more “feel good” days than symptomatic days? Are you able to function and complete tasks personally and professionally without your health getting in the way?