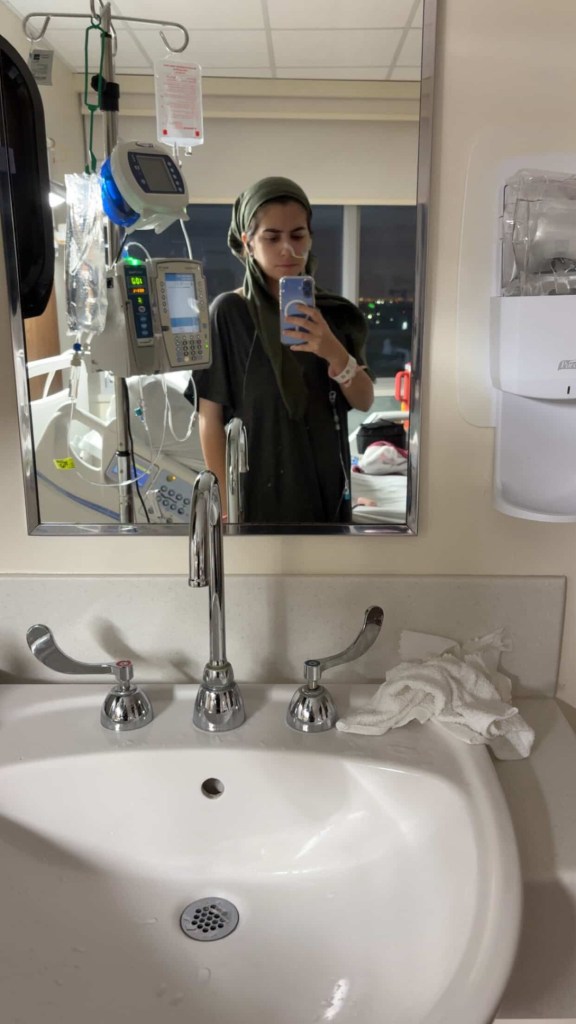
When you live with Inflammatory Bowel disease, there’s no telling if or when you’re going to need an NG tube (nasogastric tube) to help stabilize your symptoms, deliver nutrition, and help your body heal. In my 20-plus years living with Crohn’s disease, and despite many hospitalizations for bowel obstructions, I have never needed one (yet). Recently, a fellow IBD mama on Instagram shared about getting one as she’s hospitalized right now (with a new/additional diagnosis-Gastroparesis), and her experience inspired this article.

This week on Lights, Camera, Crohn’s, a guide that breaks down what to expect, what helps, and how we can best cope from fellow patients and caregivers who have lived through it. Whether you are facing your first tube placement or supporting someone who is, the fear of the unknown can often feel bigger than the procedure itself.
Understanding the Process (and Why It’s So Intense)
NG tube placement can feel overwhelming because it involves an extremely sensitive area: your nose, throat, and gag reflex. It is quick, but not exactly pleasant. Knowing what is coming can dramatically reduce anxiety.
An NG tube is typically used for:
- Bowel rest and decompression during IBD flares
- Relieving bowel obstructions
- Nutrition support
- Medication delivery
And while the experience varies widely, preparation and honest communication with your care team make a huge difference.

Before Placement: Preparing Your Mind and Body
- Ask for numbing options: Most hospitals can use lidocaine spray or gel in your nostril to make the initial insertion more tolerable. It is worth requesting.
- Practice slow breathing: Focusing on deep, steady inhales through your nose helps decrease the gag reflex and keeps your body relaxed.
- Sit upright with your chin slightly tucked: This position straightens the path the tube travels and can make the process smoother.
- Have emotional support: Whether it is a partner, parent, friend, or even someone on speakerphone, having a familiar voice can ease anxiety.
During Placement: Strategies That Actually Help
- Swallow as the tube advances: If the nurse allows, sipping water and swallowing as the tube moves downward helps guide it into the esophagus rather than the airway.
- Anchor your eyes on one spot: A visual point of focus reduces the instinct to pull back or panic.
- Choose a mantra: Something like “This is temporary” or “Every swallow gets me closer” can center your mind.
- Ask your nurse to narrate the steps: Knowing what is happening and when it will be over prevents surprises and makes the process feel more controlled.
What Patients and Caregivers Have to Say
Hindy: “I would say to request the thinnest tube possible. It is really awful.”
Ashley: “It’s a horrible experience. I’m glad I didn’t know what to expect before getting one placed, because I don’t think I would’ve been able to handle it. I don’t think there’s anything that could have prepared me for it.”
Amy has IBD and her four-month-old daughter does not, but she has had an NG tube for two months, due to issues with strength, stamina, and desire to eat after being born prematurely.
“She was diagnosed with Failure to Thrive, and her NG tube has been lifesaving! I can guarantee she gets the nutrients she needs to grow and thrive. She tolerates the NG tube very well. She has pulled it out multiple times, but thankfully we live close to the GI clinic and a great Children’s hospital.”
Amy has found there are certain strategies to limit the number of times she pulls the NG tube out, such as taping it closer to her nose. She says it can be stressful at times, but luckily with her medical background she knows how to clean the tube 8 times a day. Even though her daughter has handled the NG tube like a champ, Amy and her husband have decided to transition to a G-tube, since their baby girl will need nutritional support for a little bit longer, which Amy thinks will aide in comfort and speech development.
Alexis: “Get a little white board so that you can write what you want to say as talking is so uncomfortable.”
Karen: “Taking anti-anxiety + pain medication to help with the uncomfortable pain and anxiety that NG’s cause. I refuse NG tubes now without serious meds, the trauma, pain, and discomfort they cause must be treated and I think providers really underestimate how traumatizing it is to have one, especially if it’s put in while you’re awake.
Amanda: “Ask for some nebulized lidocaine before insertion.”
Abbie: “Ask for throat numbing spray!!! I was given it my first time and then every other time I’ve had to ask, but I’m so appreciative the first nurse I had gave me some so I knew to ask for it in the future.”
Sarah: “I didn’t even know what an NG tube was until it was already inserted. I suppose the shock of how quickly the insertion went shielded me from the pain and discomfort. Numbing spray was the only way I could cope with the tube irritating my throat. Mine was in for three days while I had a bowel obstruction and the day it came out felt like FREEDOM.”
Becca: “They are the f***ing worst. You can quote me.”
Melissa: “I had one they put in while I was awake and after SIX tries, I was adamant on getting something to relax me. They put a little something in my IV and then it went down without an issue. I also had a smaller one, more child-sized than adult.”
Dana: “I wish I had something positive to say about NG tubes, frankly I didn’t cope at all until they gave me Ativan and eventually a muscle relaxer. Sometimes they can give you a numbing throat spray to help with irritation. After the first few days, it gets little more tolerable as your body gets used to it.”

Jennifer: “OMG. 26 years with Crohn’s and nothing traumatizes me more than the mention of an NG tube. I was about 95 pounds the first time I got one. I’m almost 5 feet tall, and after two tries of me not being able to breathe they realized I needed a child-size tube.”
Mayara: “When I had my NG tube, I used to suck on ice chips/cubes to help ease my sore throat.”
Claire says she’s been through the wringer with NG tubes. There was a point where she had 10 in one year!
She says, “Regardless of how awful NG tubes are and the damage (long or short term) they can do, they have saved my life repeatedly. I am no stranger to bowel obstructions. Developing strictures seemed to be a favorite past time for my small intestines. The NG tube is supposed to decompress the obstruction and stop or at least reduce the amount of vomiting (also helps to prevent aspiration). I will never forget how nervous I was before my first NG placement and even now as an NG vet, I still get very nervous. I always ask the doctor for IV Ativan or IV Valium beforehand.


Claire also says even if a doctor does not want to give a benzo after an opiate that they will usually give her a dose right before placement.
“Don’t be afraid to ask for what you need. I also won’t sugarcoat it; you will most likely gag and vomit during the placement. Ask for an emesis bag or basin. It sounds counterintuitive, but if the nurse doing the placement is experienced, they will be able to utilize you gagging/vomiting to get the tube in faster. Nosebleeds are also very common.”
After NG Placement: Getting Comfortable
- Secure the tube well: Do not be shy about asking for gentler tape, extra adhesive, or adjustments. A well-secured tube is less irritating and less likely to tug.
- Soothe nasal irritation: Saline spray, warm compresses, or a tiny amount of water-based lubricant around the nostril can reduce soreness in the first day.
- Experiment with sleeping positions: Many find sleeping slightly elevated or on their back with a supportive neck pillow helps keep the tube comfortable.
- Be comfortable: Wear loose tops, zip-up hoodies, or scarves if you want to conceal the tube and prevent snagging on straps or bags. Obviously, many people are choose to stay in their hospital gown.
- Protect it in the shower: A bit of cling wrap or a small waterproof dressing keeps the tape from falling off.
- Move with intention: Sharp head turns or bending forward quickly can tug the tube and cause discomfort. Slow and steady helps.
Support for Caregivers: What Helps Most
As a caregiver, it can be easy to feel helpless on the sidelines as you watch your child or a loved one or friend go through this. Here is how you can help ease that burden:
- Watch for tension or kinks: If the tube starts pulling, the patient may feel nausea or pressure.
- Track symptoms: Be mindful of any changes you may notice with coughing, reflux, or fullness. This can mean the tube has shifted.
- Learn how to flush the tube: If this is a long-term situation, educate yourself so you can help prevent blockage and avoid urgent care visits.
- Offer emotional space, not pressure: Let your loved one set the tone. Everyone is different. Some want distraction, others want quiet, some want humor. Follow their lead. You know them best, trust that instinct and know that even if they may seem frustrated or short, that anger is not geared towards you, but rather the difficult circumstance and situation they are enduring.
The Emotional Side: What We Don’t Talk About Enough
Having an NG tube can stir up fear, embarrassment, frustration, sadness, or anger. All these feelings are normal.

Many patients say:
- They feel “less like themselves.”
- They are worried about how they look.
- They are afraid to sleep.
- They are overwhelmed by the sensation of the tube at first.
These feelings tend to ease within 24–48 hours as the body adjusts. Give yourself grace. This is a medical tool, not a reflection of strength, identity, or dignity. It is ok to feel all the feelings.

Celebrate the small wins
Take this one like you do with all things IBD. Give yourself credit where credit is due! It is not easy and it is important to celebrate all the wins, no matter how “small” they may seem. You are making strides and growing through this journey, whether you realize it or not. What you are experiencing matters and your resiliency deserves celebrating!
- The first time you swallow without noticing the tube
- Sleeping through the night
- Getting out of bed more comfortably
- Tolerating feeds or feeling abdominal relief
When to Call Your Care Team
You may wonder what is “normal” and what deserves pushing the nurses light or alerting your care team. You should reach out immediately if any of the following happen:
- You have trouble breathing or persistent coughing
- The tube appears to be slipping out
- There’s significant nasal bleeding
- You feel intense nausea or vomiting
- The tube becomes clogged and flushing does not help
You should never hesitate to call. NG tubes are temporary but important, your team expects questions. Classic example of better safe than sorry. You are not a burden to anyone.

Final Thoughts
An NG tube can feel intimidating, and while extremely unpleasant, they can help give you some relief while allowing your doctor to keep finding answers for you. With preparation, the right coping strategies, and the support of a caregiver or medical team, you can make the experience more manageable. Always remember you are never alone in your fears and setbacks and that your ability to cope and your voice matters.
Additional Resources:
Tricks of the Trade: Making NG Tube Placement Less Horrendous // ACEP
The Role of Enteral Nutrition in Patients with Inflammatory Bowel Disease: Current Aspects – PMC
NG Tubes for IBD: Video and Tips for Swallowing
Nutritional Support Therapy | Crohn’s & Colitis Foundation
Tube Feeding | My Experience with a Nasogastric Tube for Crohn’s Disease | Let’s Talk IBD


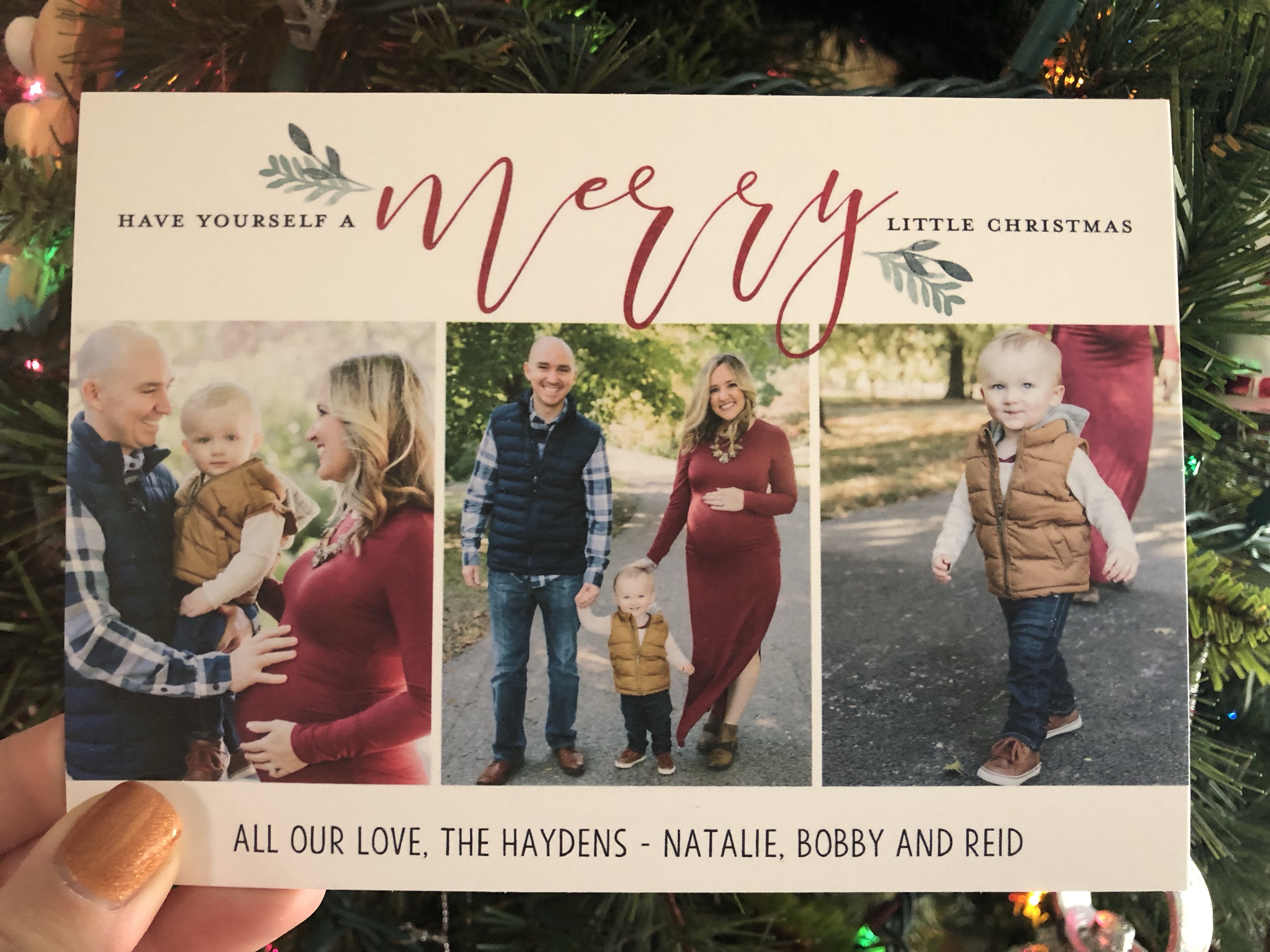
 I never dreamed I’d be walking around a toy store looking for gifts to comfort and distract my cousin’s darling, smiley, 21-month-old son. But here we are.
I never dreamed I’d be walking around a toy store looking for gifts to comfort and distract my cousin’s darling, smiley, 21-month-old son. But here we are. When we got the call March 19th that my cousin Nicole’s sweet boy Lukas was diagnosed with ALL (acute lymphoblastic leukemia) my mom and I let out deep guttural cries. It felt like an out of body experience. The tears poured down our faces. Life stopped in that moment. My husband had to run our 23-month-old son upstairs so he wouldn’t witness our despair. Our boys are only eight weeks apart. Our boys were supposed to have a play date two days later. But now, sweet Lukas was getting chemo in the hospital instead.
When we got the call March 19th that my cousin Nicole’s sweet boy Lukas was diagnosed with ALL (acute lymphoblastic leukemia) my mom and I let out deep guttural cries. It felt like an out of body experience. The tears poured down our faces. Life stopped in that moment. My husband had to run our 23-month-old son upstairs so he wouldn’t witness our despair. Our boys are only eight weeks apart. Our boys were supposed to have a play date two days later. But now, sweet Lukas was getting chemo in the hospital instead. In the blink of a moment—she went from having two perfectly healthy sons—to finding out her baby was in for the fight of his life. A fight that would involve 3.5 years of chemotherapy. A fight that would involve countless nights in the hospital, setbacks, highs and lows with dire consequences, and having to watch your child take on the beast that is cancer.
In the blink of a moment—she went from having two perfectly healthy sons—to finding out her baby was in for the fight of his life. A fight that would involve 3.5 years of chemotherapy. A fight that would involve countless nights in the hospital, setbacks, highs and lows with dire consequences, and having to watch your child take on the beast that is cancer. She held her baby tightly, sobbing in silence as he looked around the room, unaware of the poison getting pumped through his veins. It killed me to see her go through this. It’s truly the unthinkable to watch someone you love hurt so badly as they take on the unknown.
She held her baby tightly, sobbing in silence as he looked around the room, unaware of the poison getting pumped through his veins. It killed me to see her go through this. It’s truly the unthinkable to watch someone you love hurt so badly as they take on the unknown. He’s going to give life a whole new perspective. He’s going to thrive. Lukas is going to navigate these unknown waters and open our eyes to the beauty of a feel-good day.
He’s going to give life a whole new perspective. He’s going to thrive. Lukas is going to navigate these unknown waters and open our eyes to the beauty of a feel-good day.
 I hope you take this week to enjoy time with loved ones, relax and find time to care for yourself!
I hope you take this week to enjoy time with loved ones, relax and find time to care for yourself!