When you think of ostomy, what comes to mind? As someone whose had Crohn’s for more than 15 years, but never been an ostomate, it’s something that has loomed over my head since diagnosis. I’ve always wondered if I would ultimately end up with a bag and what that would mean for my life. I know I’m not alone in those worries and curiosities. Which is why I’m kicking off a 4-part series on Lights, Camera, Crohn’s— “So, You Have An Ostomy.” Over the course of these articles you will hear from more than 20 ostomates from around the world.
Today—we’ll focus on what it’s like to find out you need an ostomy, the complexity of coping, and adjusting to your new normal.
What it’s like to wake up from ostomy surgery
Blake Halpern, 39, of Texas, was diagnosed with ulcerative colitis in November 2004. By April 2005 he had a temporary ileostomy. After four weeks of being hospitalized on full bowel rest, it was determined he would need his colon removed. Blake says he was so worn out and emotionally drained, he felt like a shell of his former self. He was anxious to have the surgery and get his life back on track.

“The ostomy is so shocking. It seems like something out of a Sci-Fi movie. My small intestine poking through my abdomen emptying my waste into a bag?? That’s crazy. But it gave me some semblance of my life back. I was able to get out of the hospital, slowly start eating again and reclaiming my life.”
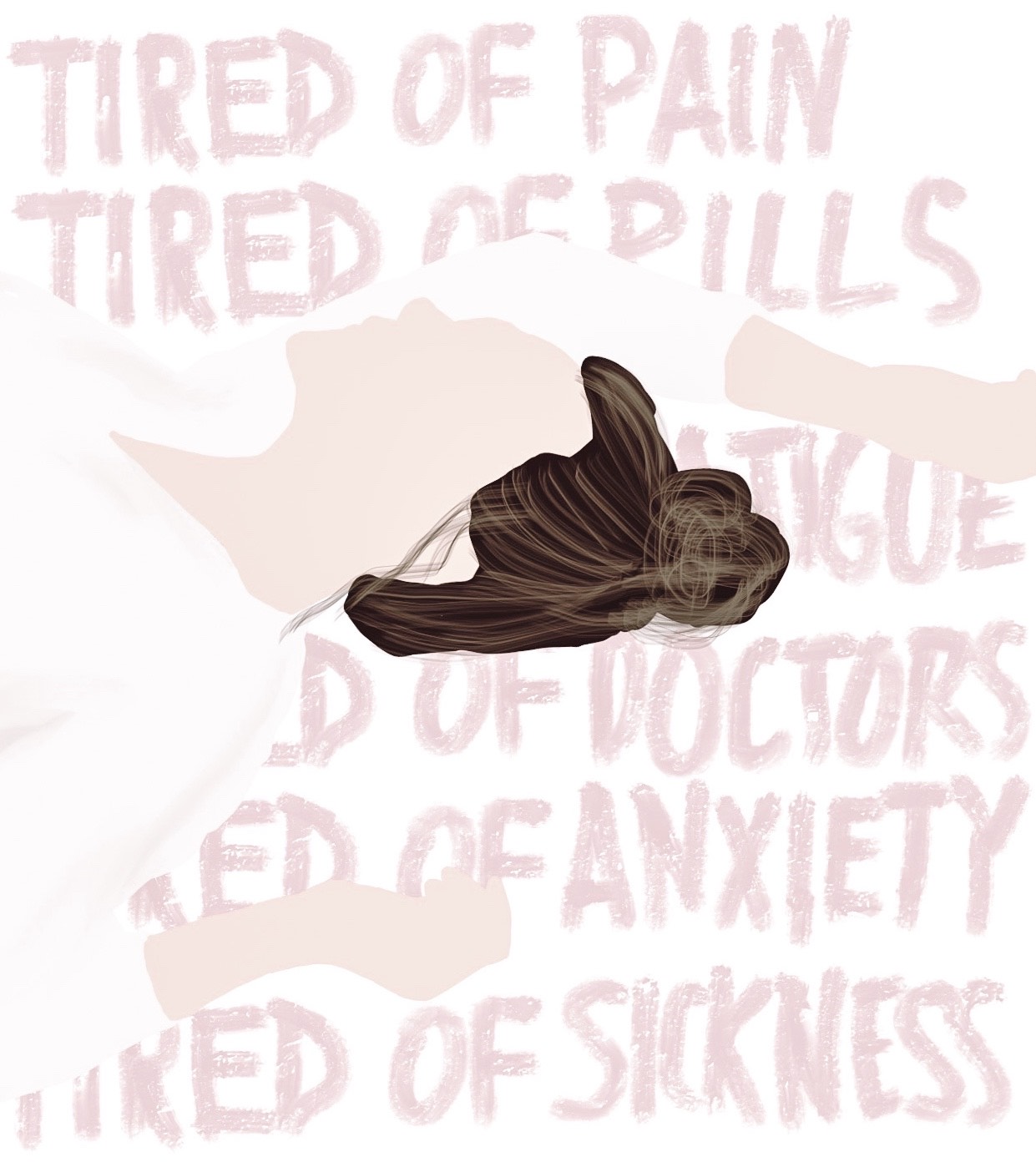
Alison Rothbaum, 41, of Ohio, was diagnosed with Crohn’s disease in 1994 at age 15. She says prior to her ostomy surgery, she went into a very dark mind space that she wasn’t prepared for.

“I woke without a pivotal organ. I woke with a new prosthetic device attached to me. I ached in my belly and in my heart. I needed to mourn the loss of the organ. It’s hard to describe unless you’ve experienced it. I refused to look at myself from the top to bottom in the bathroom mirror for a week. I didn’t want to see what the new body looked like, even though I had already begun to learn how to change my ostomy while lying in my bed.”
For Tina Aswani Omprakash, 36, of New York, needing an ostomy struck a major chord for not only her, but her family. She recalls how her dad hated his ostomy while he was alive and used to rip it off when he was in a coma in the hospital. Because of that, her mom had a significant amount of PTSD from his experiences and was against Tina receiving one. Her cultural society also told her that no one would marry her or accept her if she was an ostomate.

“I held off for as long as I could, but I started thinking that an ostomy wouldn’t be as bad as everyone was saying. I knew I needed to listen to my heart and to my doctors. My gut feeling (as flawed as my gut may be) was right. My ostomy had become my baby so to speak and I grieved for months if not years for the life it had given be back. Don’t let society sway your thinking. Seek counseling and ask all the questions you can to your surgeon and Wound, Ostomy, and Continence Nurse (WOCN) before the operation so you can feel a bit more at ease.”
Tina recommends connecting with fellow ostomate online over social media and through blogs. She says an ostomy doesn’t have to be a life sentence, but rather a life-saving force.
Adjusting to the new normal
Renee Welch, 34, of Toronto, Ontario was diagnosed with Crohn’s when she was nine years old. Getting an ostomy was a life or death decision for her. She knew the life she was currently living wasn’t what she was destined for and ultimately the choice was out of her hands.

“The hardest part of having an ostomy was recovery. It’s a long process that is not progressive. Mine took three months until I was able to feel like myself and even after that my energy was not the same until six months down the road. Recovery is something you can try to mentally prepare for, but you never know.”
Natasha Weinstein, 28, of Connecticut was diagnosed with Crohn’s at age 11. She can still remember feeling that tug on her skin and not knowing if the bag was going to randomly fall off. Eight years later, she’s still impressed with how strong the adhesive is! One of her main struggles was adjusting to her new self-image.

“No longer would I have a “flat” right side when I looked in the mirror, in fact I was always going to have this device protruding and as a college student and a young adult that’s a lot to adjust to.”
Payge Duerre, 21, of Iowa, was diagnosed with ulcerative colitis in 2003 at age 5. Her advice—not to think of your entire life as the first couple months after surgery.

“The first couple months can be shitty. More pain, more recovery, less muscle, new foods, new clothes. The entirety of ostomate life is not like that. My first three months post op were spent relearning life. But now I’m two years post op. I’ve already re-taught my body, but I’m always constantly learning new tips or tricks from other ostomates to make life easy.”
Advice for those who need an ostomy
Ashley Clark, 27, of British Columbia, was diagnosed with Crohn’s when she was 19. Her main piece of advice, “If you’re at a point where you are contemplating ostomy surgery, get it sooner rather than later. Waiting until getting my ostomy was a matter of life or death is one of my biggest regrets. It took me so much longer to recover because I let myself get so sick before I would agree to it. Looking back, I think, wow my life is so much better now, if only I had known it would be and agreed sooner.”

Tionna Forchion, 32, of New Jersey, was diagnosed with Crohn’s when she was 13 years old. She ended up getting an emergency colostomy after a bowel obstruction, so she wasn’t able to mentally prepare for the everything that came her way. Tionna says she was angry at first and cried for days, but as time passed so did her acceptance for how having a bag saved her life.

“My advice for anyone on the verge of getting a bag or needing one is that there is life after getting an ostomy. So many times, people say they don’t want a bag because they assume there will be so many things they can no longer do and that is so false. You can still travel, swim, go to college, have kids, get married and do everything a person without a bag can do.”
Gaylyn Henderson, 36, of Atlanta, Georgia, was diagnosed with Crohn’s at age 14 and has a permanent ileostomy. She says at times with chronic illness you can’t help but wonder if there is anyone out there who really understands what you’re going through, but that there is.

“You need to meet them, and you need to seek them out to know that what you are feeling is not unusual. The feelings you have are very real and it’s not out of the ordinary to be feeling that way. You are not crazy, your life is. There is an importance to building a fellowship of those that can relate to what you are going through. It is imperative to know you are not alone. You may not go through the exact same circumstances, you may not have the same diagnosis, but chances are you have similar experiences and can relate more than you realize. You need to know that what you are going through you will get through.”
Stay tuned for Part 2 of “So, You Have An Ostomy…”, Wednesday (September 23rd) we’ll cover diet recommendations, how to pack when you’re traveling, and how best to change your bag.







































 His disease had gone unmonitored for years and his new doctor was performing a colonoscopy to see just how bad his IBD had gotten. We were unaware that he had developed a stricture that was so severe that when she pushed the scope through, it nicked the wall of his intestines, causing a perforation and bacteria to get into his bloodstream. Within 45 minutes of waking up from the procedure, he had spiked a 104-degree fever and kept telling me and the nurses he thought he was dying. I was TERRIFIED. But I also found myself motivated by the fear and the anxiety I felt.
His disease had gone unmonitored for years and his new doctor was performing a colonoscopy to see just how bad his IBD had gotten. We were unaware that he had developed a stricture that was so severe that when she pushed the scope through, it nicked the wall of his intestines, causing a perforation and bacteria to get into his bloodstream. Within 45 minutes of waking up from the procedure, he had spiked a 104-degree fever and kept telling me and the nurses he thought he was dying. I was TERRIFIED. But I also found myself motivated by the fear and the anxiety I felt.