Crohn’s disease and ulcerative colitis often require medication to keep inflammation under control, but in some rare circumstances, just one medication isn’t enough. Research shows only 40 percent of people with IBD achieve remission within one year of taking a single drug. Dual Targeted Therapy (DTT) involves using two different types of treatments at the same time to achieve better disease control. This disease management plan comes to play when single-drug therapy does not adequately control symptoms or when a more aggressive treatment is needed.
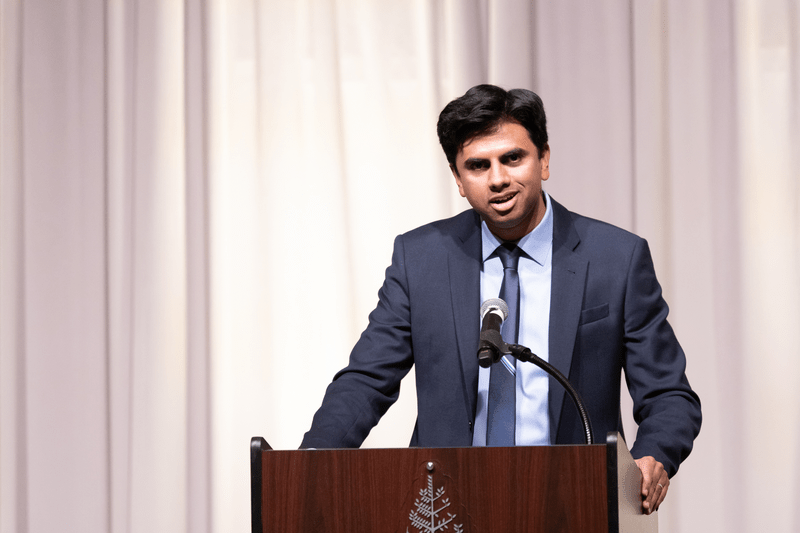
This week on Lights, Camera, Crohn’s we hear from esteemed gastroenterologist Dr. Laura Targownik along with several IBD warriors who have utilized DTT to help manage their IBD.
IBD Dual-Targeted Therapy Options
There are several ways healthcare professionals can help manage IBD with dual therapy.
Biologics and Immunomodulators
More commonly, combining a biologic therapy such as infliximab (Remicade), adalimumab (Humira), or vedolizumab (Entyvio) along with an immunomodulator like azathioprine, 6-mercaptopurine, methotrexate. The purpose of this is to enhance the effectiveness and potentially lower the risk of developing antibodies against biologic drugs.
Biologics and Small Molecule Inhibitors
A newer approach involves combining a biologic with a small molecule inhibitor like tofacitinib (Xeljanz) or upadacitinib (Rinvoq). This can target different pathways of the immune response, potentially offering a more comprehensive approach to suppressing inflammation. This can be used in refractory cases and should only be prescribed by an expert IBD physician.
In patients who do not respond to single biologic therapy, there is growing interest in using two biologic agents targeting different inflammatory pathways. However, this approach is not yet widely supported as healthcare providers weigh side effects risks and this is considered experimental.
Dr. Laura Targownik, MD, MSHS, FRCPC, Mount Sinai Hospital (Toronto), Departmental Division Director (Gastroenterology and Hepatology), University of Toronto gives a case study for when she would consider using two biologics for example: in a person with fistulizing Crohn’s disease, whose fistulas have responded well to biologic therapy, she would consider adding another biologic if they’re still experiencing inflammation in the intestinal lining. Dr. Targownik says medications such as vedolizumab (Entyvio) or an IL-23 such as risankizumab (Skyrizi), mirikizumab (Omvoh), and guselkumab (Tremfya) could help to bring IBD under control.

“As a gastroenterologist, I don’t want to discontinue the anti-TNF because I fear their fistulas will worsen, so it makes more sense for me to add in a well-tolerated biologic like vedolizumab or an IL-23 to try to bring the luminal disease under control,” said Dr. Targownik.
She went on to say that patients support the idea of combining therapy with different mechanisms of action if the safety profile makes sense. Most patients who are in a position where dual therapy would be considered are open to do what it takes to get their disease under control.
Corticosteroids and Other Immunosuppressants
This is not strictly speaking dual therapy because corticosteroids are always used short-term. But prednisone in conjunction with other immunosuppressants can quickly reduce inflammation while waiting for the slower effects of immunomodulators or biologics to set in.

A Look at DTT and IBD Research
Dr. Targownik says the VEGA and EXPLORER clinical trials shed light on the potential benefits of combining biologics.
The VEGA trials looked at the benefit of combining an anti-TNF (golimumab) and an IL=23 inhibitor (guselkumab) to induce remission in people with moderate-to-severe UC.
“The combination of golimumab and guselkumab outperformed monotherapy, with a 15 percent increase in the likelihood of clinical remission and a 20 percent gain in endoscopic response. Patients then received an additional six months of either golimumab or guselkumab monotherapy,” says Dr. Targownik and the group on the dual treatment had higher rates of improvement and remission.
This suggests that the deep remission obtained early through DTT might have a sustained effect, even if you step down to monotherapy.
“The EXPLORER-CD study was an open label trial looking at high-risk patients early in the course of disease,” says Dr. Targownik. They received a triple combination with adalimumab, vedolizumab, and methotrexate for six weeks. By the end of the study, 55 percent were in clinical remission, and 35 percent were in endoscopic remission. As there was no comparison arm, it is not clear whether these rates are higher than what would be expected.”
Consequently, the use of tumor necrosis factor (infliximab , adalimumab, etanercept, and golimumab) in combination with newer agents which target interleukin (IL)-12 and IL-23 (ustekinumab, UST), a4b7-integrin (vedolizumab, VDZ) or a4-integrin (natalizumab), has become an increasing area of interest in patients with disease that is not responding to treatment.
According to a systematic review looking at the efficacy and safety of DTT, “There is an urgent need to optimize treatments for patients” so that they have a better chance of remission, which unfortunately remains unachievable for a large number of people living with aggressive IBD. More research is needed to evaluate what the optimal drug combinations are, as well as dose and frequency to limit the burden of side effects.

The DUET trials are looking at people with Crohn’s disease and ulcerative colitis, much like the VEGA study, to compare the effectiveness of golimumab + guselkumab versus either drug alone. Interestingly, in this study, golimumab and guselkumab are combined in a single medication, so even though there are two active ingredients, it is delivered like a single drug.
“If we limit our discussion to combinations of modern advanced therapies, the combination of an anti-TNF and either vedolizumab or an IL-23 holds the most promise,” Dr. Targownik says. ”The other combination that we are seeing more is combining a JAK-inhibitor with an anti-TNF for people with acute severe UC, where the JAK-inhibitor is used in addition or in place of a corticosteroid trial.”
Personal Experiences on DTT
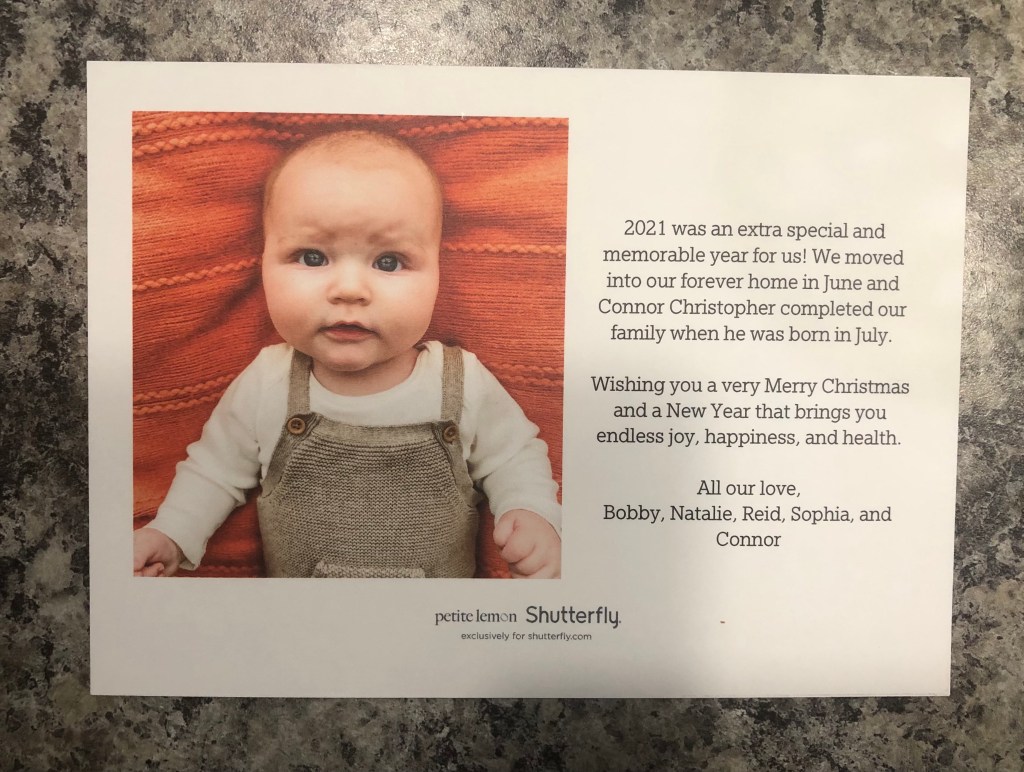
I’ve lived with Crohn’s since 2005 and luckily have been on the same biologic since 2008. I ran an Instagram poll that asked, “Have you been on dual-targeted therapy for your IBD?” Of the 320 people who responded, 40 percent said “Yes”, and 60 percent said no. Here are some scenarios they share:
Candyce has managed her Crohn’s with infliximab (Inflectra) and azathioprine since 2020. A 10-day hospital stay led her to dual treatment therapy after she received the recommendation from both her rheumatologist and her gastroenterologist. “My GI wanted to try to wean me off the azathioprine in 2022 after a clear colonoscopy, and I flared to the point of her wanting to hospitalize me,” she says. “But I managed to gain remission with prednisone and getting back on azathioprine, along with increasing my Inflectra dose to every six weeks instead of every eight.”
Risankizumab wasn’t doing the trick on its own to control Brad’s IBD, so his GI added 28 days of Rinvoq as an alternative to prednisone. He says, “This really worked wonders. Being on both risankizumab and Rinvoq put me into biochemical remission in less than 60 days.”
Samantha’s daughter, Eloise, was on tofacitinib and vedolizumab prior to her colectomy.She shares that more families are talking about dual therapy options. “The major issue is getting these medications approved from insurance, especially for pediatric patients. Our doctor was able to get us samples of Xeljanz from a local adult gastroenterologist because insurance would not approve it.”
Kate currently takes vedolizumab and upadacitinib to manage her IBD. Previously, many biologics failed her and vedolizumab was the only one that worked, but it did not address her perianal disease. “The Rinvoq is beginning to work,” she says. “However, I will say it caused awful acne (which I’m now on medication for). I’m not out of the woods yet, but I am functioning again, and I can tell that two medications are working on what needs to be healed.”
Courtney has been on Remicade and Azathioprine since 2020, prior to that she was on Humira and Azathioprine. She says, “I had no reservations because I was sick and willing to accept any option that might bring relief. My doctor explained to me that Azathioprine helps prevent antibodies to biologics. Regular blood tests monitor for more serious concerns.”
Along with her Remicade infusions, Lauren takes methotrexate orally each week.I don’t love it to be honest. I feel much more fatigued and nauseous with methotrexate added into the regimen.”
Initially, Danielle was put on azathioprine when she was on Remicade to prevent antibody formation and to help keep trough levels high. She explains, “When Remicade wasn’t working and I switched to Stelara, we decided to keep the azathioprine on since it didn’t give me any noticeable side effects. I have had some liver abnormalities with the azathioprine. So, I’ve had to have blood work and even an MRI of my liver to make sure everything is ok (it is). Now that I’m in remission with Stelara, my doctor gave me the choice of coming off the azathioprine, but I wanted to keep it on because I haven’t been in remission so long.”
Cait receives infliximab infusions, and she takes azathioprine simultaneously. “So far, I’ve noticed a massive difference in the healing of my perianal Crohn’s.”
Katie manages her IBD with Skyrizi and methotrexate. She says the combination makes her fearful at times. “I feel like it is a lot for my body to handle, and I have never been able to tell if that is a true feeling or something that stems from the thought of it. I also want to get off methotrexate within the next year or two to prepare my body for pregnancy. But this combo has provided me with full remission and the best I have felt in years.”
Final Thoughts to Consider Before Trying DTT
It’s important to discuss whether DTT could be for you with your specialized IBD care team as DTT comes with its fair share of risks and considerations. Combining medications can increase the risk of adverse effects, including serious infections due to greater immune suppression. Also, getting dual therapies approved through insurance can be complicated, making the cost and accessibility an issue for patients.

“It is challenging to get coverage for patients to use more than one advanced therapy at a time,” Dr. Targownik says, but not impossible. “Often if a patient has another autoimmune disease, I can get one medication approved for the IBD, and then the other for the other autoimmune disease like rheumatoid arthritis.”
The Takeaway
The effectiveness of combination strategies in IBD has been demonstrated in various studies, but these decisions need to be made on a case-by-case basis, considering your personal disease severity, response to previous treatments, and overall health status. If you are struggling with getting your IBD under better control with one therapy alone, speak to your IBD physician about other options.

















































 Now more than ever, we’re being labeled as the “sickly”, the “disposable”, the “weak”, the list goes on. COVID-19 is not JUST about the elderly and immunocompromised, this is about everyone. As patients we have a unique perspective and understanding about the struggles we face daily and what it’s like to go through this challenging time. Connect with fellow patients online who get your reality, your emotion, and the whirlwind of going up against this invisible bogeyman. To refrain from social media, you can download awesome free apps like Gali Health and IBD Healthline, with helpful articles, community conversations, and chats by patients, for patients.
Now more than ever, we’re being labeled as the “sickly”, the “disposable”, the “weak”, the list goes on. COVID-19 is not JUST about the elderly and immunocompromised, this is about everyone. As patients we have a unique perspective and understanding about the struggles we face daily and what it’s like to go through this challenging time. Connect with fellow patients online who get your reality, your emotion, and the whirlwind of going up against this invisible bogeyman. To refrain from social media, you can download awesome free apps like Gali Health and IBD Healthline, with helpful articles, community conversations, and chats by patients, for patients.
