Chances are you’ve heard of Pelvic Floor Therapy but may not know what this entails or why so many people in the IBD community are talking about it. Individuals with IBD can have persistent symptoms of fecal incontinence, constipation, rectal discomfort, and diarrhea, despite having their IBD in remission with medical therapy. These persistent and often debilitating symptoms can have a major impact on your wellbeing and quality of life.

This week on Lights, Camera, Crohn’s we hear from two gastroenterologists from Mayo Clinic along with several IBD warriors who provide insight, helpful guidance, and information about pelvic floor therapy.
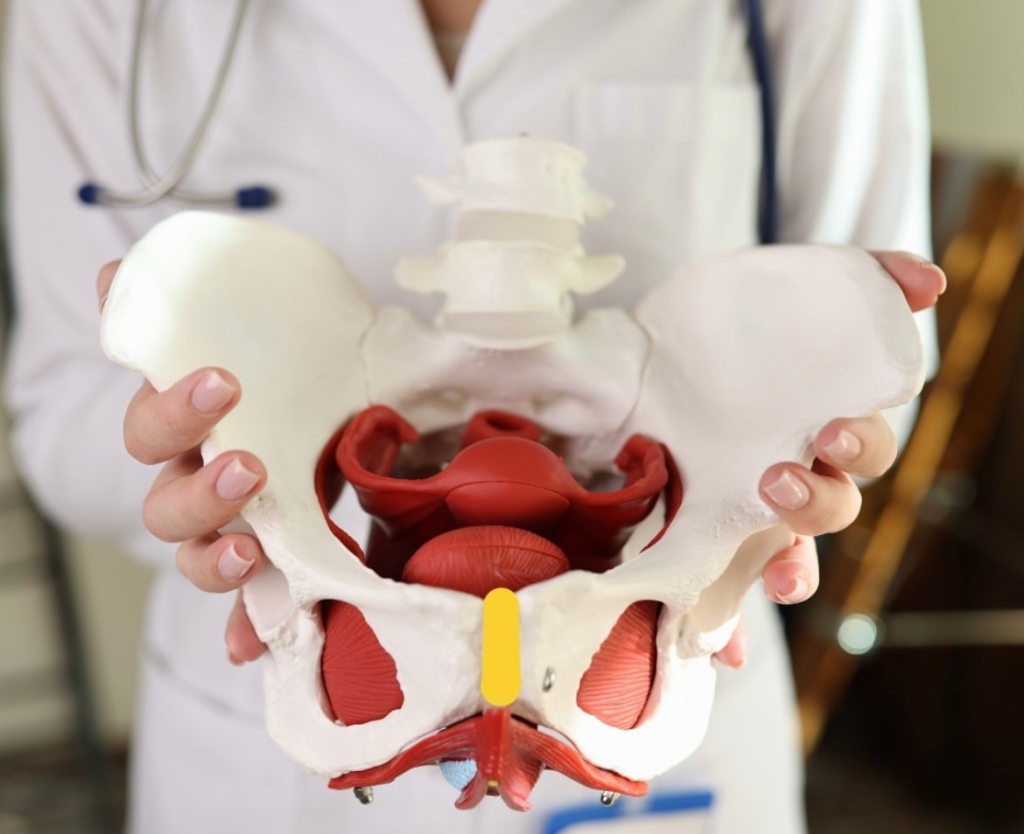
What exactly is Pelvic Floor Therapy?
Pelvic floor therapy is a treatment program performed by pelvic floor therapists to retrain the pelvic floor muscles to address underlying issues such as constipation, fecal incontinence, or urgency. Many patients with IBD in remission may develop pelvic floor dysfunction which is usually diagnosed from a digital rectal examination in combination with an anorectal manometry test.
“During an anorectal manometry, a small catheter with sensor probes and a balloon is placed into the rectum and is connected by a wire to the computer. During the test you are lying on your side and asked to perform maneuvers to determine how your pelvic floor muscles work. At the end of the test, they inflate a balloon in the rectum to help evaluate for sensation and then ask you to simulate having a bowel movement by pushing the balloon out,” explained Dr. Katie Dunleavy, MB BCh BAO, Gastroenterology Fellow, Mayo Clinic.

Based on normal values for your age and gender, you may be diagnosed with a pelvic floor dysfunction. Dr. Dunleavy went on to say that in IBD, there is less research on the benefits of pelvic floor therapy.
“But we have seen benefit in up to 80% for patients in remission who continue to have symptoms of constipation, urgency, or incontinence once active inflammation is fully ruled out. Similarly, some patients with IBD undergo total proctocolectomy with ileal pouch anal anastomosis (IPAA) may also benefit from pelvic floor therapy if they have issues emptying their pouch,” said Dr. Dunleavy.
Additionally, those with IBD who’ve had pelvic floor surgeries might experience sexual dysfunction and this type of therapy directed towards relaxation of the pelvic floor can lead to a better sexual experience.
Pelvic Floor Dysfunction does not discriminate across genders
Any person can develop pelvic floor dysfunction and may benefit from treatment with pelvic floor therapy in the right setting.
“While most studies describe pelvic floor in females, I believe individuals from all genders deserve evaluation of their pelvic floor the recommendation for pelvic floor therapy. Furthermore, individuals of a transgender experience, might undergo gender affirming surgery that impacts their pelvic floor muscles, and would benefit from pelvic floor therapy,” said Dr. Victor Chedid, M.D., M.S., Gastroenterologist at Mayo Clinic.

Dr. Dunleavy says, “As many as 50% of people with chronic constipation have pelvic floor dysfunction, which means there is impaired relaxation and coordination of the pelvic floor and abdominal muscles during evacuation. Some common symptoms include straining with hard bowel movements, a feeling of incomplete evacuation, pain with intercourse, or urinary symptoms.”
Certain risk factors make it more likely for men or women to develop pelvic floor dysfunction, this includes instrumented vaginal deliveries, chronic constipation with straining, prior surgery, prolapse, and age. It is important for men and women to discuss symptoms with their doctor to ensure they get the appropriate testing and treatment.
Apprehensive about getting looked at?
It is important for people diagnosed with pelvic floor dysfunction to seek out a qualified pelvic floor therapist who is specialized in GI and evacuation disorders. These are generally physical therapists or occupational therapists who complete extra training in pelvic floor therapy.
“You should find a therapist you trust and will feel comfortable with during your therapy sessions. The therapists who work in this area are fantastic and work diligently to explain what they will be doing. My patients tell me that the relief they feel from therapy well exceeds the apprehension they had prior to starting sessions,” said Dr. Dunleavy.

It’s important for patients to feel comfortable talking with health care providers and addressing concerns they may have on this topic. Dr. Chedid typically discusses the benefits of pelvic floor therapy with patients during clinic visits as a beneficial treatment option that does not require surgery. He provides patients with exercises and techniques to do at home that will have a major impact on general wellbeing and health.
“Individuals with IBD experience significant “negative” experience with the bathroom and with defecation that can be quite traumatizing, and therefore when they get in remission, they still have a negative association with the bathroom and might have “fear of defecation” despite being in remission. I equate that to “PTSD of the pelvic floor”, which is not a medical term, but an analogy I use. Therefore, pelvic floor therapy is essential to reverse this negative experience with the bathroom and make their bathroom experience a healthier and satisfying experience. Almost all patients who I describe this to get it right away and understand the importance of pelvic floor therapy,” said Dr. Chedid.
He adds that it’s imperative health care providers communicate with patients and ensure that the therapy session will be a safe space with at rained physical therapist who is trained in empathetic and trauma informed care. This is essential in putting a person’s mind at ease, as many patients might have experienced sexual trauma in their lifetime that makes pelvic floor therapy triggering for them.
The impact of Pelvic Floor Therapy post operatively and after IBD pregnancy
If you’ve had a total proctocolectomy and an ileal pouch anal anastomosis (IPAA), you might experience non-relaxing pelvic floor dysfunction or pouch evacuation disorder. This is similar to the rectal evacuation disorder in individuals with pouches.
“Typically, this is identified by history, physical exam, pouchoscopy, anorectal manometry and dynamic imaging of pouch evacuation. Additionally, someone who has had any form of trauma to the pelvic floor, including Perianal Crohn’s disease or surgeries for Perianal abscesses or fistulas or lacerations due to vaginal deliveries after pregnancy, these patient might experience rectal evacuation disorders after recovering and healing. In the proper patient, if identified by history, physical exam and the right testing, these patients will benefit from pelvic floor therapy,” said Dr. Chedid.
At the same time, there isn’t a lot of research on pelvic floor therapy in the post-operative state or following pregnancy in patients with IBD.

“There have been several attempts to find normal values for patients with IPAA who have undergone colectomy to help diagnose pouch related pelvic floor dysfunction. We generally recommend patients wait until the anastomosis following surgery is completely healed prior to having an evaluation with a balloon to ensure no complications. Similarly, patients who have recently undergone delivery from pregnancy will likely require time to heal. I would discuss this with your doctor to have more personalized information,” advised Dr. Dunleavy.
If your GI recommends pelvic floor therapy for your personal symptoms and struggles the overall response is tremendous.
“Recommending pelvic floor therapy to everybody, without identifying the right patient who would benefit from it is not typically beneficial. Therefore, in the right patient, pelvic floor therapy is extremely effective,” said Dr. Chedid.
What IBD patients have to say
Stacey has ulcerative colitis and went from having an ostomy to becoming a j-poucher. She’s a big proponent of Pelvic Floor Therapy. After her 3-step surgery to j-pouch in 2021, she knew she needed at least an evaluation from a pelvic floor physical therapist (PFPT) after urination became a challenge and inserting tampons became impossible during her takedown recovery.
“My surgeon wouldn’t write me a referral, citing that the anorectal manometry tests prior to surgery were all normal. My GI doctor didn’t want to go against the clinical judgement of my surgeon, so I couldn’t get one from her either, and finally I received a referral from my OB/GYN after explaining that penetrative sex was impossible (and felt unsafe to me) to even attempt,” Stacey explained.
These delays resulted in 5 months of significant pelvic pain that she felt ill-equipped and under-supported to handle, and this time could’ve been saved if she had gone into surgery with a referral to see PFPT from the get-go, even if she didn’t need to use the referral; it would’ve been nice to have.
“It’s so wild to me that orthopedic surgery has extensive PT rehabilitation protocols, and yet I was met with such resistance to gain access to the professionals who could help support my muscular recovery, even after such extensive GI surgeries,” she said.
During Stacey’s initial encounter with the PFPT, she spent the majority of the visit trying to gain a strong understanding of her entire pelvic and holistic health history, everything from sexual health to physicality to surgery, and all the in-between.
“She asked for consent prior to any invasive exams and explained them in thorough detail, reminding me that I was in control and could always choose to stop an exam if I felt unsafe. She continued to breathe with me during the exams and communicated her findings in real-time, which made me feel at ease. At the conclusion of our visit, I was told that I was experiencing hypertonic pelvic floor dysfunction from a decade of clenching for dear life trying to make it to the bathroom with mod-severe UC, even before my surgeries. The tightness of the muscles, coupled with three extensive pelvic surgeries, contributed to the pain and issues I was experiencing,” said Stacey.
During the visits with the PFPT, Stacey discovered she had no awareness of her pelvic floor muscles whatsoever. She could not distinguish the relaxation of the muscles from the contraction, and the entire area felt numb to her, like it was a holy, empty space. She says this made the exercises challenging to understand initially. She was prescribed specific exercises, not Kegels, including strategies to gain awareness of supportive muscle groups so she could begin to engage with this part of her body and start to heal.
“What I did not expect, however, was for this experience to be as enlightening and empowering as it was. Slowly but surely, the little life things showed me that they’re the big life things: being able to fully urinate in under 20 minutes, FINALLY being able to use tampons again- these were MASSIVELY important to my quality of life, and they became possible through the help and support of a PFPT and my adherence to their prescribed exercise regimen. I even realized one day while holding one of my exercise poses that I could feel the muscles DEEP in my abdomen! They felt heavy, full of pressure, as if they fired on to greet me, and then suddenly… I could feel them gently, slowly, RELEASE. I cried tears of relief realizing that I had been fearful of reconnecting with these muscle groups, and it really was safe and okay to be in my body.”
Stacey says she had NO idea these muscles existed, yet here they were. Had they been here all along?! She says she numbed them out from years of associating the deepest parts of her with pain from UC; and that her brain was protecting her. I truly wonder. All she knows is the day that she could FEEL her body experience relaxation and safety with FULL awareness of these pelvic muscles is the day that she knew that healing from these surgeries was going to be possible.
After one year of PFPT, Stacey “graduated,” not free of pain, but with the tools to know how to live within the ebbs and flows of pain. She tells me she still relies on the tools and bodily awareness that she gained through the experience.
Jessie was diagnosed with Crohn’s disease when she was 15 years old and after more than 22 surgeries later, at the age of 38, she says she completely underestimated how much her pelvic floor was affected over the years by the inflammation, surgeries, and her pregnancy.
“I was “guarding” badly (a response to pain) and so weak. I was having bladder issues, pelvic pain, rectal pain and so much more. After 2 years of being consistent going to pelvic floor therapy and doing the exercises I can say I’m about 85% better. I can’t say enough how much of a HUGE difference pelvic floor therapy made in my life and my IBD journey. My therapist explained it to me like this “you don’t have orthopedic surgery on your knee, wrist, ankle, spine, etc. and not get prescribed physical therapy. Same with an injury. It’s just standard procedure. But, for some reason, even though your pelvic floor consists of tons of muscles, ligaments, tendons, bone, etc. the same process is not considered – but IT SHOULD BE!” Your pelvic floor needs to be rehabbed after any injury, strain, surgery, etc. just like any other muscle/tendon/ligament/bone in your body,” explained Jessie.
Claire started PFPT because all imaging and tests showed that while her inflammation is under control, she still experiences extreme pain.
“I was tested, and they found I have dyssynergic defecation. This was caused by my chronic pain due to long-lasting fissures as well as chronic constipation. I’m grateful my GI thought to have me tested for this, as many don’t make that connection since the symptoms are so similar to Crohn’s. During PT, I have learned that my muscles do not relax and are constantly tense, so we work on trying to get them relaxed in order to successfully pass bowel movements. Like all other PT, one downside is that it is a lengthy process and takes up a lot of time. I have a one-hour appointment every week for 12 weeks and an hour or two of exercises and stretches on my own every day.”
She says she’s started to notice improvements and found ways to make her pain more bearable, though it’s something she will have to continue working on for a long time.
Tiffany has accessed pelvic floor therapy for herself and having previously been a physio and a fellow Crohnie, she recommends people speak with their doctors because it can make a world of difference, especially after surgery, hospitalization, or a flare.
“The neural connection we have to our trunk and pelvic muscles can be re-trained and strengthened, allowing less pain, and for me an improved sense of control over urgent bowel movements.”
Preslie was diagnosed with Crohn’s in June 2016, and after two years of battling severe symptoms, she had a colonoscopy that showed she was in remission. It may sound like lovely news, except Preslie was still living with a ton of pain, so her and her care team started digging for answers.
“This led to an Endometriosis diagnosis in August 2018. That was great news, except I STILL was not getting relief, and started having severe burning anytime I urinated, but always tested negative for UTIs. I went to a male urologist who told me I was just constipated, which was not the case. After well over a year of extremely painful sex, constant pain, and burning when I peed, I went to a urogynecologist who talked with me for less than 10 minutes and had the diagnosis: Interstitial Cystitis and Levator Ani Syndrome. I finally felt heard. I started pelvic floor therapy shortly after and immediately felt relief.”
Rocio says pelvic floor therapy was recommended to her by a home health physical therapist who was treating her for neuromuscular issues after bowel resection surgery for her Crohn’s in 2020.
“During my resection recovery, I was struggling tremendously with constipation, which was unfortunately always my issue with my IBD. Although uncommon, it’s been my reality for the last 20-plus years. The reason I share this is because I wish someone would have recommended pelvic floor therapy to me over all those years.”
She began seeing a pelvic floor therapist in January 2021 and completed two years of treatment. During that time, Rocio says she learned a lot about the intricacies of all the muscles, the nerves, the internal blood flow, and so much more. Because of two fistulotomies and a stricturplastly, she has numerous anatomical issues which prevent her from having normal bowel movements.
“Pelvic PT changed that completely and I have normal/formed BM’s every single day, without any signs of constipation and without any straining. I’ve learned ways in which I can help relax and release the pelvic floor should I face issues in the future.”
Separately, Rocio has learned how beneficial pelvic floor therapy is for many IBD patients post-operatively, including the ileal resection she had. Her therapist worked on her abdomen significantly during appointments to prevent adhesions and scar tissue. She says there are so many benefits to pelvic floor therapy that it does make her wonder why more IBD health care providers aren’t encouraging patients to pursue care.
Annie started pelvic floor therapy two weeks ago. She was referred based on suspected interstitial cystitis, not her IBD. She was shocked to learn during her first appointment that treatment was for all conditions that involve urgency of any kind.
“The game changer was the pelvic exam itself, I never realized what my PT noticed right away, which is that my first layer of pelvic muscles are unnaturally sensitive. This is massively helpful for IBD and IC, but the most validating part was having a lifetime of excruciating intercourse and painful pap smears and knowing the reason. My PT told me this is not how my life has to be. After just two weeks of exercising my pelvic muscles with a vaginal wand and daily targeted yoga, my urgency, both with my Crohn’s and IC, has gotten so much more manageable. I started this journey running to the restroom every 30 minutes (even at night), now I feel like I’m starting to get my life back.”
Jasmine says pelvic floor therapy helped her a ton following j-pouch surgery.
“I truly believe it should be integrated into post-op care plans, I had to seek it out and ask for it.”
Amy says that while she doesn’t have experience yet with PFPT, she has a complicated Crohn’s history for the past 25-plus years. Now that she’s over 40 and has had three vaginal births, she recently asked her doctor about pelvic floor therapy.
“Because of all the IBD women sharing their journey with this on the Internet, it inspired me to look into therapy for myself. In my first request, the response was that it might be a fantastic idea, but to wait and see. My next visit is in a couple of weeks and I’m looking forward to utilizing this article to share and take with me to help me advocate for myself.”
A look at the insurance piece
Yes, pelvic floor therapy can be covered by insurance, but it can vary based on the type of insurance. It is also important to ask about coverage for biofeedback therapy which is an essential part of the therapy based on prior research studies. Many insurance companies will need proof of diagnosis using an anorectal manometry with balloon expulsion test or defecating proctogram.
“If the proper indication based on testing is identified with the referral to pelvic floor therapy with a script written by someone’s GI provider, then typically insurance should cover it,” said Dr. Chedid.
Closing thoughts on Pelvic Floor Therapy and IBD
It is important to discuss with your doctor if pelvic floor therapy is right for you. Once patients with pelvic floor dysfunction have these basic tools, they can begin retraining the pelvic floor muscles with biofeedback. Biofeedback provides auditory and visual feedback to help retrain the pelvic floor and relax the anal sphincter. Biofeedback training is the treatment of choice for medically refractory pelvic floor constipation, with some studies showing improvement in more than 70 percent of patients. Patients also learn to identify internal sensations associated with relaxation and long-term skills and exercises for use at home.
At Mayo Clinic patients have had more than 70% response at 3 months following initiation of pelvic floor therapy. The response usually takes weeks to months to see a clinical difference and requires patients to practice their exercises and biofeedback at home.
“Although many centers are familiar with retraining techniques to improve pelvic floor dysfunction, few have the multidisciplinary expertise to teach patients with constipation how to appropriately coordinate abdominal and pelvic floor muscles during defecation, and how to use bowel management techniques, along with behavior modification, to relieve symptoms. Because pelvic floor dysfunction can be associated with psychological, sexual, or physical abuse and other life stressors, psychological counseling is often included in the evaluation process,” said Dr. Dunleavy.
If you have chronic pain, you may also need to see a physician to have these issues addressed prior to starting pelvic floor therapy.
Key takeaways from fellow IBD patients
- PTs are an excellent resource, but just like getting an IBD-ologist is superior to a general GI doctor, PFPTs are an even stronger resource, ESPECIALLY in the context of chronic GI disease where so many of our deepest muscles are constantly working on our behalf.
- You can always say “no thanks!” You don’t need to agree to any sort of exams or exercises that you’re not ready for, and a compassionate PFPT will empower you to make decisions and communicate in alignment with your body’s needs.
- ANYONE can benefit from PFPT: any age, any gender.
- Normalizing pain and discomfort is a survival instinct, but it’s not necessarily serving you for the GOOD life- it’s okay to get evaluated if you’re concerned about sexual pain or dysfunction, pain with periods, or if you also have IBD and simply want to be sure that you’re supporting your pelvic and spinal muscles the best you can so that you can, especially in the bathroom!
- YOU get to decide! Having an evaluation may be all you have the capacity for, and that’s okay! You can return for a plan of attack later, or you can wait until you have the capacity to dive in head-first! There’s no one right way.
- If you decide while talking to a PFPT before they do ANY manual evaluations that something doesn’t feel right- YOU GET TO CHOOSE, and you can always, always say, “nevermind”. Advocating for your body is always progression in your healing journey, every single time.
- SPEAK UP! It’s RIDICULOUS that patients have to ask and ask and ask for the bare minimum, but if it helps your quality of life and it’s within your capacity- it’s certainly worth it.
- A big deterrent for patients can be cost, but the investment is worth it, if you can swing it. You would be surprised how much every system of your body is so connected and feeds off one another!
Helpful resources to check out
- Find a Pelvic Floor Therapist Close to Home
- Utilize the “Section on Women’s Health” or the “Herman & Wallace” websites. Both these groups train therapists who specialize in pelvic floor disorders.
- The Section on Women’s Health (SOWH) website has a “PT Locator” tab. You can enter search criteria including your geographic location (e.g., zip code) and specialty (e.g., constipation) to identify a therapist closer to home.
- The Herman & Wallace website has a “Resources” tab under which you will find a “Practitioner Directory.” Use the map features to locate a therapist near you.
- Utilize the “find a provider” section of www.pelvicrehab.com for a local PT by zip code.
- The therapists who work with pelvic floor disorders may be in Gastroenterology, Urology, Gynecology, Physical Medicine, and/or Women’s Health, etc. You may be able to find someone through your local physicians or contacts.
For those in Canada, check out the Canadian Physiotherapy Association. It has a “Find a Physiotherapist” tab which allows you to connect with the sites of participating provinces/territories. By specifying a “Women’s Health” therapist or equivalent, you may find someone who specializes in the field of incontinence, pelvic pain, constipation, etc.
The benefit of pelvic floor therapy also involved patient education, relaxation exercises, diaphragmatic breathing, and correction of maladaptive toileting behaviors. Some studies have shown improvement in quality of life relating to symptoms, and mental health.
Biofeedback in patients with ileoanal pouch dysfunction: A specialist centre experience
