It’s safe to say every prep for a colonoscopy is a shit show. The show just looks a bit different each time. I completed another annual colonoscopy this past Friday, and the process still keeps me on my toes, even after more than 17 years of living with Crohn’s disease. As those of us with IBD know, it’s so much more than the prep. It’s the anxiety of wondering if our disease is active. It’s the worry about whether our IBD is going to act up and be triggered by the ungodly amount of laxative we are ingesting in one sitting. It’s the fear of going through more trauma getting an IV and dealing with nurses and a care team we’re unfamiliar with. It’s resenting the fact that you’re a young person needing a colonoscopy…and the list goes on.
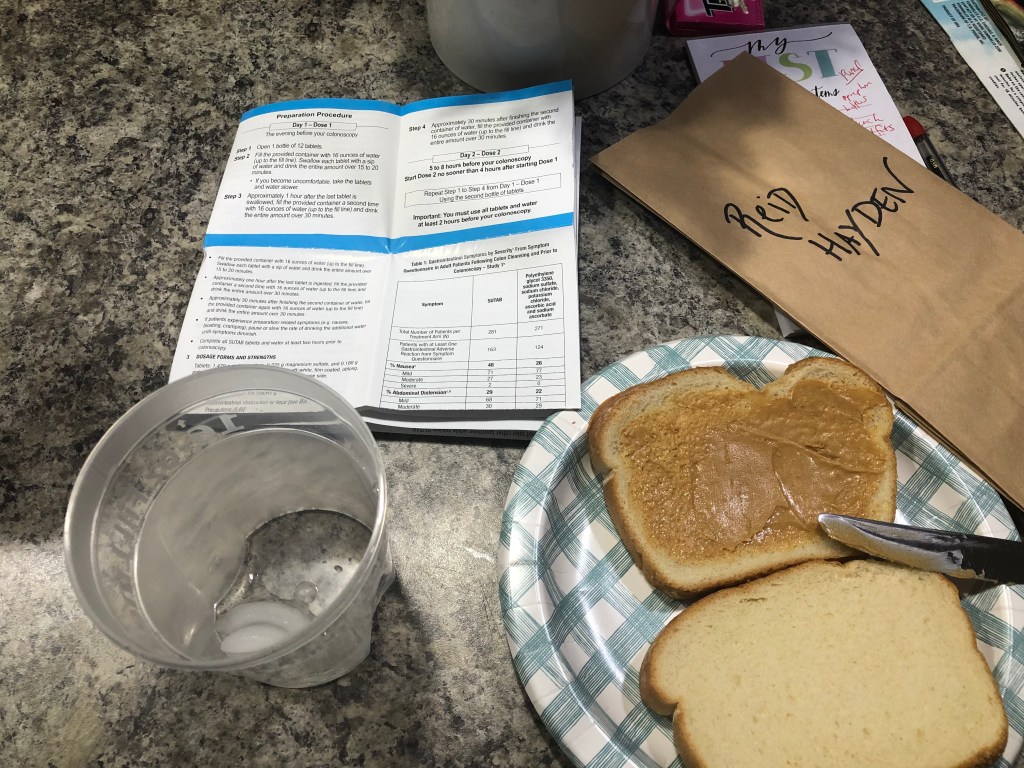
I did my second-ever pill prep (SUTAB) this time. I find swallowing 24 pills to be easier than guzzling anything that tastes unpleasant. There was a bit of a monkey wrench in my game plan this time around, when my gastroenterologist’s nurse informed me over the Patient Portal that magnesium citrate saline is recalled. Because of that, my doctor created an additional prep to make up for that. For some reason, the 24 pills deemed worthy for the rest of society to take to get cleaned out isn’t good enough. I received instructions two weeks prior to my scope that quite frankly scared the bejesus out of me.

Along with the 24 SUTAB pills and 96-plus ounces of water, patients are expected to:
- Take 1,500 to 1,600 mg of magnesium citrate pills, twice (This adds 12 pills to the prep, and they are horse pills)
- 30 ml of Milk of Magnesia
- Two enemas…yes, you read this correctly.
…the moment I received this news, my chest tightened, and I started to freak out. Regardless of the prep you choose (you’re “allowed to choose any one you like:”) …this is also “required”. Knowing this ahead of time made my mind race and I kept going back and forth about whether I was going to put myself through it or be my own advocate and go a bit rogue. It’s a bit daunting when the instructions are in CAPS and there’s the threat of needing to do everything over again.
Here’s what I did for my prep
It’s easy to talk a big game and say “there’s no way I’m doing this” …but at the same time, there’s a worry that looms that if you don’t, you may need to do another scope because you aren’t cleaned out enough. I’ve always been a bit of a rule follower, so it tends to take a lot for me to go against the grain.
I always do a self-imposed liquid diet to give me some buffer in case I encounter issues with the prep. My last meal is generally the Sunday night before a Friday scope. I allowed myself some crackers on Monday night, but other than that, I was strictly liquids all week. It’s brutal, but it always pays off in the end.

I bought magnesium citrate pills, the SUTAB pills, and the fleet enemas. I didn’t bother getting the Milk of Magnesia.
I took the first 1,500 mg (6 pills) of magnesium citrate, starting at noon the day before my 11:30 am colonoscopy. To me, it was a lot easier doing the pills than having to drink an entire bottle of magnesium citrate, which immediately causes me to vomit. I then timed out the 12 SUTAB pills, by setting a timer on my phone. I took one every 2-3 minutes. All you do is take the pills with 16 ounces of water and then follow that with drinking 16 ounces of water two more times over a couple of hours. I was “done” with my prep by 4 pm the day before my scope and wasn’t running to the bathroom too much.
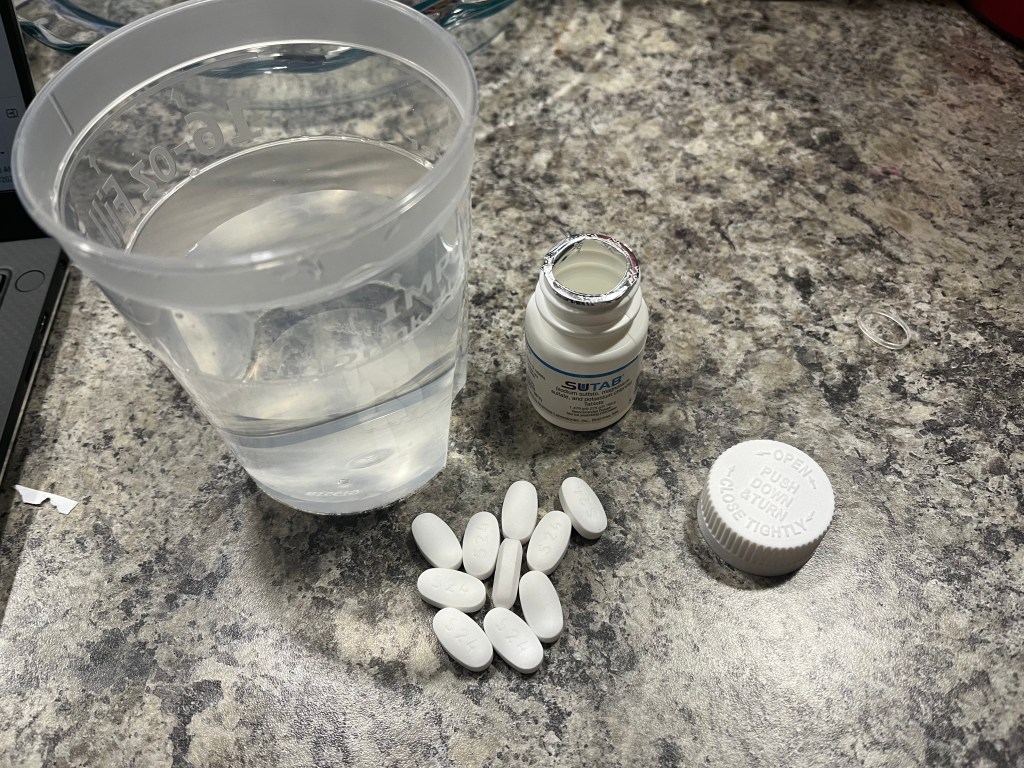
I went to bed and set my alarm for 5 a.m. with the intention of doing the other 12 SUTAB pills + the additional 6 magnesium citrate. At this point, I was still on the fence about whether I would try an enema.
I walked downstairs in my dark house as my family slept and turned on a few lights so I could lay all the pills out on the kitchen counter. It was just me—all these enormous pills—and my thoughts. I got the 12 SUTAB down and after about 30 minutes I started feeling ill. I ran to the bathroom and vomited quite a bit…at the end I puked up bright red blood. It was petrifying. I screamed for my husband while I was on my hands and knees on the bathroom floor at 6 am. He ran down the stairs and could see how much anguish I was in. I immediately called my mom who is a nurse and she told me not to take anymore pills and that my prep was done.
My mom, who lives out of town, has been with me for every single prep since diagnosis, but this time around, she wasn’t since it’s so close to the holidays. Not having her by my side added a bit to the stress. I asked her if I should do the enema and had some choice words. She told me not to do it. I agreed. Hospitals are running low on enemas right now, so the instructions said to “bring an enema to the hospital in case you need it.”
Speaking up prior to the procedure
My scope wasn’t until 11:30 a.m., unfortunately it was very busy at the hospital, so I didn’t get mine until 1:15 p.m. When you haven’t eaten in nearly a week and your head is pounding from dehydration, every minute feels like an eternity. When the nurse finally got me from the waiting room, we got to the endoscopy suite and while I was still in my street clothes, she asked me if I had my enema with me. I froze in my tracks. I told her I forgot it on my counter (I purposefully forgot it on my counter) …and I proceeded to go into an explanation about how ridiculous it is to expect this of patients, how unnecessary and over the top it is and that I refuse to do it. She asked me if I did the enema earlier in the morning, I said no. To my surprise, she completely empathized with me and said she couldn’t agree more that it’s making all their procedures run late, that no other GI’s require it, and that she knows after 17 years with Crohn’s I know what I’m doing. She was whispering in cahoots with me, and it felt SO good to feel validated and heard.
When I told her I had difficult veins, rather than rolling her eyes or downplaying my fears, she listened and was so kind. She took a close look at all the options and ended up choosing a vein in my right hand. She got me with the first stick and immediately all my anxiety around the IV went away.
I informed my GI and anesthesiologist that I had vomited blood while doing the prep. They let me know that was from throwing up and it caused the capillaries in my esophagus and stomach to break and bleed. Because of that I was told prior to my procedure that in the event there was blood down below, an endoscopy would also need to be performed. Luckily that was not the case! I was given an antacid in my IV to help resolve any possible issues. I made the mistake this time of not taking my prescribed Zofran to prevent nausea. If you have a history of vomiting with prep, I highly recommend getting a script and taking this 30 minutes prior to starting your prep. In the moment, I was already taking so many pills I didn’t feel like adding one to the mix, but I wish I had.

The colonoscopy results
When I woke up from that amazing propofol nap I was thrilled when my GI gleefully walked into the recovery room with a huge smile on her face and told me that my small bowel and colon were “pristine”, that everything looked gorgeous, and that I was still in remission. The discharge notes state there is “normal mucosa in the entire examined colon” and that my “end-to-side ileo-colonic anastomosis” (where my small intestine was reattached to my large intestine from my bowel resection surgery in 2015) is characterized by “healthy appearing mucosa”. No biopsies were taken and the “quality of the bowel preparation was excellent”.
Remission is a complicated term and one I don’t take lightly. I reached surgical remission in 2015, after a decade of ups and downs. While I’m so grateful to continue the 7-year-streak of remission, I’m aware that tomorrow things can change. All any of us can do is focus on the right now and try not to dwell on what could be or what can happen. Remission is just a word—I didn’t do anything to deserve it, no one does. So much emphasis can be placed on being in remission, and I get that it can feel like a big deal—but IBD, whether you’re in “remission” or not is unpredictable, so there’s no sense in thinking you’re in the clear or invincible just because you’re told you’ve reached it. Remission does not mean you are completely free of symptoms.
My tips for going through a colonoscopy
- Schedule your scope during an early time slot. Not only does this allow you to eat a lot sooner, but you’re also more likely to be taken right on schedule and not face any delays. For my 11:30 a.m. scope, I wasn’t at a restaurant until 3 p.m. I will say as an IBD mom, the 11:30 a.m. time was ideal in the fact I was able to get my two older kids ready for school and drop offs had already taken place before my husband and I left for the hospital.
- Arrange childcare as you’re scheduling your scope. It’s challenging as an IBD mom or dad to have to worry about who is going to take care of your kids during procedures. Get the available dates for your colonoscopy and figure out childcare as you’re scheduling so there’s one less moving piece to deal with. My mother-in-law watched our kids from 9:30 a.m.-4:30 p.m. and it was comforting to know I had nothing to worry about while my husband and I were away.
- Add in some buffer with a liquid diet for a few days. I’m not saying you need to go crazy with the liquid diet, but even doing one extra day of liquids will really ease your prep when it comes to what you need to pass. It also gives you a bit of leverage if things don’t go as planned when you’re trying to get it all down.
- Listen to your body and do what you’re comfortable with. While there are guidelines and recommendations if you are vomiting, feeling sick, struggling to make it through the prep, just do what you can. Don’t push yourself to the brink of putting your health at risk. The SUTAB pills specifically say “Do not take other laxatives” … so how is a patient supposed to feel when their GI tells them to do a laundry list of additional laxatives?! The general population does the prep, without any add-ons. We should be able to do the same. I had to chuckle when I was told my prep was excellent, when I went off the grid and did what I felt was best. Before my procedure I smiled at my doctor and told her I did my best…and that’s all they can ask for.
- Get labs ahead of time. The past few years my care team has tried to save me a trip to the lab and tried to get lab work through my IV. Each time, it’s been a nightmare. Last year the nurse in recovery stuck me 8 times and I was so dehydrated she never got any blood. She was unkind and rough and left me in tears. That was it for me. This year, I did labs the Monday before my scope. Having that checked off my ever-growing patient to-do list eased my anxiety and the nurse who did my IV said because she didn’t need to get labs through my IV, the needle could be a lot smaller—score!
- Count the pills. I noticed this time I was given one extra SUTAB pill in my prescription bottle. I triple counted to make sure. There should be 24, total. Make sure not to take any extra.
- Be cognizant of the time of year you get your scope. Get tests and procedures done prior to the end of the year when you’ve most likely reached your deductible, so you save money. I have a bone scan scheduled this week as well, crossing everything off the list when it’s covered.
- Always remember gummy bears are a liquid. I share this year after year but so many people still seem unaware that this is the case. The day prior to a scope you need to steer clear of red and purple gummy bears, but you can eat gummy bears throughout a liquid diet and the day before your scope. The ability to chew something and have something sweet is a gamechanger. It’s a great way to chase prep that doesn’t taste good, too. This time around my sweet daughter took it upon herself to take all the red gummy bears from the bag so I wouldn’t accidently eat one…she made a pile of red gummy bears and proceeded to eat all of them.
- Check about patient savings options. SUTAB is a bit pricier than other preps, you can save by going to http://www.sutab.com and printing off a coupon that brings the cost down to $40 with most insurances. Look into this regardless of what prep you do to make sure you’re not overpaying.
- Feel empowered in what you’ve endured. Going through colonoscopies with IBD is not for the faint of heart. Chances are you have your own routine and know what works for you. Stick to it and speak up if something doesn’t sit right with you. Plan that post- scope meal ahead of time and reward yourself afterwards. You’ve been through a lot and deserve to recover and rest.
Til next year…