If it’s happened to you, you know the feeling all too well. When I received a letter in the mail informing me that the biologic injection, I had been on for 16 years was no longer going to be covered, my stomach flipped, and my heart sank. When you live with a complicated disease like Crohn’s or ulcerative colitis and find a therapy that keeps your health in check and your IBD well-controlled, it’s extremely stressful and daunting to face the worry of being forced to switch your medication to a biosimilar or a different biologic all together.
Like many patients, I asked my gastroenterologist to appeal the forced medication switch. Even though I was almost positive we would be denied, I did not want to go down without a fight. As expected, within days of my GI’s appeal, we were told by insurance that Humira would no longer be covered and that I would need to choose a biosimilar or a different drug class all together moving forward.

I chose to go on the biosimilar Hyrimoz for many reasons—the first being that anti-TNF drugs have worked well for me for YEARS, by choosing to go off it and switch to a different drug class, I ran the risk of building up antibodies and possibly not responding as well to treatment. I also have a comfort level with self-injections and know how I have typically responded to anti-TNF medication in the past.
The emotions and heartache of having to say goodbye to a medication that carried me through for 16 years, allowed me to bring three healthy babies into this world, and stay out of the emergency room and hospital since becoming a mom 7.5 years ago tore me apart. I sobbed. I stressed. I was anxious.
Switching to a biosimilar—the emotional and physical toll
Much to my dismay, I started Hyrimoz in July 2024. The first eight days I felt the same and then my health began to crumble. I lasted four injections—and during that time I went from being in deep remission for years to needing pain medication to make it through elementary school PTO meetings and while coaching my kindergarten soccer team. I went from feeling well most of the time to running to the bathroom 15+ times a day and almost having accidents in public. I went from being able to eat whatever I wanted to worrying about how consuming anything was going to make me feel. I spent nights curled up in pain and days feeling bloated and on edge about whether every decision I made was going to make me unwell.
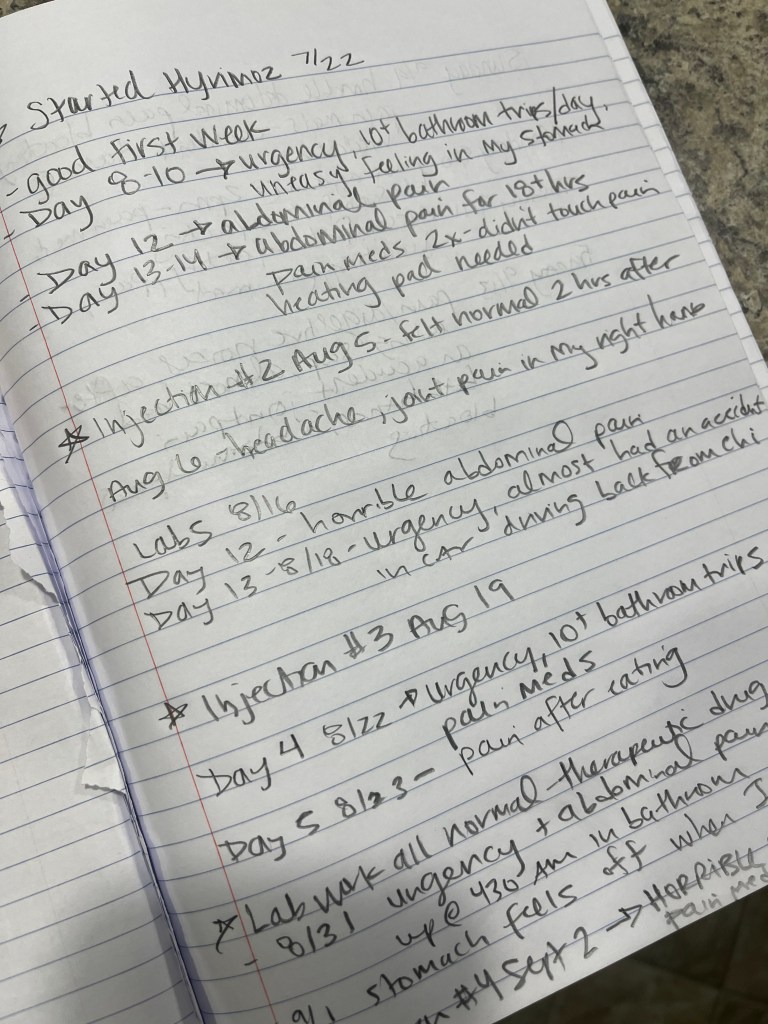
I knew something had to change. I refused to have my quality of life ripped from me without speaking up. I kept a detailed journal every single day since I started the biosimilar. I articulated my concerns to my care team repeatedly over the Patient Portal. We ran extra labs, I did a telehealth appointment, I spoke with GIs around the United States I have come to know and trust through my patient advocacy work. My care team told me that meeting in person for a clinic appointment or over telehealth would help build our case, as that carries more weight than just communicating over the Portal. Keep that in mind.
This week on Lights, Camera, Crohn’s I offer tips for building your case, writing your appeal letter, and making sure your voice is heard. Patients are constantly made to feel less than. It’s all about the profits and not about the patients. This needs to stop. Insurance companies and specialty pharmacies need to stop making our lives so damn difficult and start to recognize the havoc they cause by delaying treatment, blocking treatment options, and forcing us to change a medication that finally controls our disease. Living and managing chronic illness is a full-time job in this country. The hours and days wasted and spent on the phone dealing with all the red tape is an absolute nightmare, and unless you’ve experienced it, you have no clue the headaches it causes, the time suck it is, and how it puts the quality of our lives in jeopardy.
Keeping track of it all
When living with IBD, the bad days come and go and oftentimes we forget just how often or how horribly we feel because our “normal” is not normal. By journaling or writing in the Notes app on your phone anytime anything with your health is awry, this helps paint a clear picture for not only you, but your providers. If you can say, “On Tuesday, September 24th I went to the bathroom 10 times, I couldn’t eat, I had joint pain in my hands, and abdominal pain that required a heating pad”—this illustrates the complexity of your symptoms. Imagine having that type of intel for two months. These details help your appeal in a big way. My IBD Nurse told me that she believes my typed-out symptom journal made all the difference in winning our second appeal.
So, take notes and be as descriptive as possible. If you have a random headache and you’re not sure why, write it down. If you get new pain, you haven’t experienced before keep track of it. If you eat and must run right to the bathroom or start feeling pain jot it down.
Many of my symptoms I’ve dealt with since switching to the biosimilar feel exactly like a Crohn’s flare. After weeks of this, I started to freak out that I was losing my remission all because of a forced medication switch. A world-renowned GI took the time to call me as I was making dinner for my family one night to hear more about my situation. He did this out of the goodness of his heart to provide additional guidance and support. After hearing more about my situation, he believed it was my body having adverse side effects to the biosimilar rather than a Crohn’s flare, since my labs were checking out fine. Everything started to make sense. While he wasn’t sure our appeal would be granted, he listened and empathized with what I was going through.
Writing your own appeal letter
My IBD team recommended I also write a patient letter that they would include with their second appeal. I was happy to take the time to offer my voice and share what the experience of being on a biosimilar was like for me. At the same time, I had never written an appeal letter. Before I started I did my research on how to approach and craft the wording.
I made sure not to come off angry or accusatory. I kept the letter as professional as possible, while also explaining very clearly how horribly I was responding to the medication. I backed up my letter with science and attributed research that’s been done regarding biosimilars. I learned from research published in the Journal of Crohn’s and Colitis (2020) that while around 80% of patients have a seamless transition, 10-20% have a negative response. It’s important to note that just because you are switched to a biosimilar, does not mean your health will deteriorate. Many people thrive and don’t notice a difference, but the issue is—you don’t know how you are going to respond. I went into the transition with an open mind and as positive as possible, but the unknown looms over and it’s emotionally draining to constantly wonder if you are going to feel unwell because of the forced switch.
Tips for expressing yourself in the appeal letter
I will use Humira as an example since that was my experience, but this goes for any biologic/medication.
- Start with basic information—your name, date of birth, insurance ID number, and the policy number.
- Provide the name of the medication you’ve been switched from (in my case Humira) and the one you’ve been switched to (Hyrimoz).
- Mention the date when the change was made.
- Clearly state the purpose of the letter. For example, “”I am writing to formally appeal the decision to switch my Crohn’s treatment from Humira to Hyrimoz.”
- Briefly provide an overview of your health history with IBD, diagnosis date, and the treatments you’ve tried, hospitalizations/surgeries. If you’ve been on the same treatment for years and it’s helped you, highlight how effective the therapy has been. Mention the stability you’ve achieved with Humira—humanize your story. For instance, “While on Humira I was able to work full-time, have three healthy pregnancies and babies, and be a mom without my health holding me back.”
- Reference any previous experiences with other medications that may have failed you or caused side effects.
- Emphasize the risk of switching medications after long-term success. For IBD patients, changing medications can result in loss of response, worsening of symptoms or disease progression, potential adverse reactions.
- Have your gastroenterologist provide their own letter that emphasizes the risks of switching, the stability you’ve achieved, and their professional recommendation. They will reference any studies that are available and be able to provide medical records showing your history on the medication.
- If applicable, reference and cite insurance company policies that include provisions for medical necessity, or any pre-authorization that was previously approved.
- Emphasize the impact on your health and finances and highlight the potential cost to both your health and your insurance provider if switching leads to disease flare ups, complications, hospitalizations, or the need for additional screenings, scopes, or treatments.
Close with a strong, respectful request. End the letter with a clear statement, such as:
“For the reasons stated above, I respectfully request that you reconsider your decision and allow me to remain on Humira as prescribed by my doctor.”
I signed my letter:
My family deserves more and so do I.
Sincerely,
Natalie Hayden

Ironically, when I wrote my appeal letter I was dealing with horrible abdominal pain, lying in bed with a heating pad.
Finding out we won the appeal
Once my appeal letter and journal of symptoms were finalized, I sent them to my GI and IBD nurse over the Patient Portal. I was on pins and needles wondering what was going to come next. I sent over the materials on a Friday morning and the following Monday, I received word from my nurse over the Portal that the insurance denied the 2nd appeal because back in June when my GI submitted the first appeal, he deemed it “urgent”—in doing so, the insurance company considers those appeals “2nd level appeals”—if those are denied, they consider the case closed. Imagine that— “closing a case” before a patient has even started a different medication. Makes sense…right?! Can’t make this stuff up. When I heard this, I felt incredibly defeated.
My care team was unaware of that and asked for a clinician to review our materials—the insurance company agreed and said there would be a decision in 72 hours. That same night, while I was making dinner for my family, I received an email from CVS Specialty pharmacy saying my prior authorization for Humira had been approved. I couldn’t believe my eyes. I’ll never forget how it felt to see those words and read that email.
My kids happened to be standing around me and I couldn’t help but scream and jump and dance with tears running down my cheeks—I yelled, “MAMA’s GOING BACK ON HER MEDICINE!!!!!” I grew up in Chicago…and for any Chicago Bulls fans from the Michael Jordan days, my celebratory jump was reminiscent of what Jordan did when we beat the Cleveland Cavaliers in 1989 and he pumped his arm over Craig Ehlo.
My kids all smiled and laughed and danced with me, no idea what was really going on. But the celebratory moment was so incredibly jubilant they were smiling ear to ear. These last two months they’ve witnessed me unwell way too many times. It’s a side of my Crohn’s I’m not sure they even knew existed prior to now.

This past Friday night the same abdominal pain I’ve been dealing with began as the kids got off the bus. I had to take a pain pill before an advocacy call that was ironically about How to Deal with Insurance—for an upcoming panel discussion at a medical conference I’m speaking at in December. After my call and rushing through a makeshift meal, I took all three of my kids to my son’s soccer practice and told my friends on the sidelines how sick I felt. I came home and had to take another pain pill, had difficulty with the bedtime routine, and laid on the couch with a heating pad. But it helped to know these shitty days will hopefully be ending.
Looking to the future
This blog article is coming out the same day as I go back on Humira after winning my insurance appeal. While it’s a big win for me, it’s a small win for our community because at the end of the day an incomprehensible number of people are forced off their medications or denied off-label dosing, all so insurance companies see a better bottom line. As patients we can’t stand for this. Medical providers should and need to have the FINAL say in what medications their patients are on and they should always be willing to go to bat for their patients and appeal even if they “know they’ll get denied.” I hear all too often from fellow patients that their GI won’t even appeal in the first place and does not empathize with the fear of being forced on a biosimilar.
For those providers, I ask…can you guarantee, 100%, no doubts whatsoever that your patient will thrive and do just as well on a biosimilar as they did their originator biologic? Does the benefit really outweigh the risk? Should IBD patients who already live with an unpredictable and complicated chronic illness have to endure the stress, medical trauma, and anxiety that result from forced medication switches or denials related to off-label dosing?
As patients, caregivers, and medical providers we are a team. We know what’s right. Doctors and nurses should not have to waste so much energy on fighting for off-label dosing, necessary treatments, and keeping their patients on medications that are working. A HUGE thank you to all the providers and nurses who go above and beyond and out of their way to fight for us and do everything in their power to make sure we receive the medical treatments we need to keep our IBD in check. Your efforts, whether successful or not, are not going unnoticed.
At the end of the day, the big argument is all about “accessibility” and “cost savings” in the United States, but are patients really reaping this benefit here? I paid at most 0-$5 for Humira injections, I paid $0 for Hyrimoz. Do you know how I paid? I paid with living more than two months with health issues that would bring the average person to their knees. I went from being in deep remission to re-living the trauma of how unpredictable life with IBD can be. I paid by being on a biosimilar for 71 days and spending more than half of them with debilitating pain and symptoms.
Big pharma can step up to the plate and lower their absurd pricing on biologics (originator drugs) so that biosimilars are of no monetary benefit to pharmacy benefit managers. Let’s make it an equal playing field and see what happens. Would Big Pharma rather lose all their patients because their biologic is being removed from the insurance formulary or keep patients, lower their costs of the drugs, and keep insurance companies from choosing biosimilars because it saves them money?
As a vocal IBD patient advocate and leader, I understand and feel for those who haven’t been able to go back on therapies or receive different dosage recommendations they depend on for their well-being. While I’m thrilled to be back on my biologic, now I have the worry about whether my body will respond the same as it did previously.

The medication I’ve depended on for 16 years to bring me comfort is finally back in my fridge and going to be back in my body today. The prior authorization lasts one year, so I’m not sure what the future will bring, but I’m focused on getting my health back on track right now and worrying about that later. I’m grateful my energy in dealing with my own appeal is over and now I can pour my efforts into trying to drive change for our community. We all deserve so much more. Let’s go after what is right and make forced medication switching and off-label dosing delays and denials by insurance companies illegal in the United States.