This post is sponsored by the Autoimmune Association. All thoughts and opinions shared are my own.
An educated patient is an empowered patient. Over the weekend the Autoimmune Association presented its Inaugural Autoimmune Summit that aimed to do just that. The virtual two-day event featured 23 educational sessions and more than 50 autoimmune experts including physicians, nurses, policy experts, and of course, patient advocates.
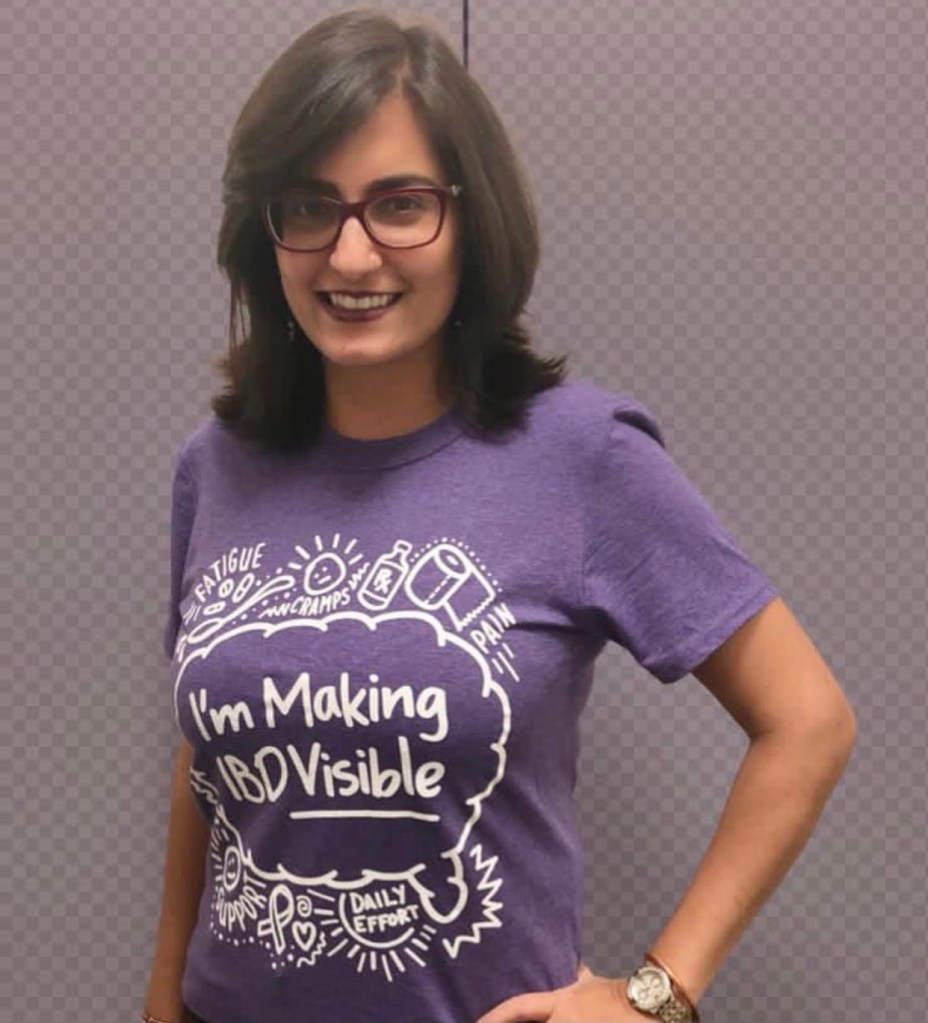
The Summit covered a wide variety of important topics that impact patients and caregivers who live with autoimmune conditions. I had the opportunity to moderate a panel discussion about fertility, family planning, and pregnancy alongside Dr. Marla Dubinsky, Chief of Pediatric Gastroenterology at Mount Sinai and Co-Director of the Susan and Leonard Feinstein Inflammatory Bowel Disease Clinical Center and Mariah Leach, a mom of three who lives with Rheumatoid Arthritis and Founder of Mamas Facing Forward. As an IBD mom of three chidren myself, I’m extremely passionate about sharing guidance and support for fellow women on this subject.
During the discussion, Dr. Dubinsky touched on many aspects of the journey to motherhood and beyond with IBD, but one comment she made resonated with me. She said the greatest gift a woman can give their child, is to stay on their medication, and allow their baby to thrive in an uninflamed environment. As someone who needed and depended on my biologic with all three of my pregnancies that comforted me greatly and really struck a chord.

Other topics of discussion during the Summit included tips and tricks for managing multiple specialists to clinical trials, health equity, advocating on Capitol Hill, and complementary medicine.
A dream come true
Lilly Stairs, Vice Chair of the Board of the Autoimmune Association and Summit Lead, lives with Crohn’s disease and arthritis. As a patient advocate, she understands the vital importance of providing those who live with chronic health conditions to share their voice and articulate their needs and struggles.
“It has been a dream of mine and the Autoimmune Association’s to plan an event that unites community members from across autoimmune conditions. Our patient odysseys share deeply rooted similarities. By coming together, we can accelerate autoimmune education, awareness, advocacy, treatment, and someday, cures.”

Goals of the Summit
The goals for the Summit were three-fold. Organizers and presenters like myself hope you walked away feeling connected to people across the patient community, while learning tangible tips for managing your autoimmune conditions. Lastly, the hope is that attendees and Summit participants feel energized and excited about what the bright future holds for those living with autoimmune diseases.
Lilly went on to say, “Events like the Autoimmune Summit are essential engagements for patients and caregivers to participate in. These events provide tools to navigate life with chronic illness and empower patients with the knowledge they need to be “CEO, secretary, and treasurer of your care” as Hetlena Johnson, Lupus Patient Advocate so eloquently stated in the Managing Multiple Autoimmune Conditions panel.”
Events like this are a reminder that we are not alone in our journeys. Even though chronic illness can be extremely isolating, events like the Autoimmune Summit offer the opportunity for connection that often feels like much needed chicken soup for the soul. The camaraderie that is possible even though Zoom has a lasting impact on helping to lift the burden and self-doubt many patients face.
From the Speakers
Tina Aswani Omprakesh participated in a panel on complementary medicine and autoimmunity. As an ostomate who juggles Crohn’s disease, Gastroparesis, and IBS, she knows firsthand how imperative it is to take on illness with multiple approaches.
“This is an important subject that’s often not discussed in the autoimmune space. The reality is that many patients are thinking about exploring it but don’t know how to navigate it in a way that can help complement their existing therapies. These conversations are essential to proliferate both credible information and sources of complementary therapies so patients can truly live their best lives possible.”
Molly Schreiber lives with Type 1 Diabetes, Rheumatoid Arthritis, and POTS. During the Summit, she spoke about what it’s like to manage multiple autoimmune conditions.

“Anytime I can share my story, my hope is that attendees feel less alone in their battle with chronic illness. We may have different health conditions, but our fight is often the same—pain management, medical providers who listen, and affordable medications we can easily obtain.”
Alisha Bridges is a patient advocate who lives with Psoriasis. She participated in a breakout session geared towards dermatology. She says having the chance to speak at the Autoimmune Summit was an honor.

“I hope my story helped viewers to better understand the unique challenges of living with psoriasis as a woman of color especially in the clinical trials sphere. These conversations are imperative to elicit change for better care of patients of all backgrounds.”
Curtain Call
It’s our hope attendees discovered tips for managing autoimmune disease from patient advocates like myself who understand your reality, while also learning about the latest research and future treatments on the horizon.
Did you miss tuning into the first-ever Autoimmune Summit? No worries! All the presentations were recorded and will be shared in the weeks ahead. I’ll be sure to share the Fertility, Family Planning, and Pregnancy discussion I was a part of on my social media channels as soon as the video becomes available.
Thank you to all who tuned in, to all who participated, to the organizers, like Lilly, and the generous sponsors who made this happen. It’s amazing to see what’s possible when patients have a proverbial seat at the table alongside medical professionals and digital health companies. Our voices matter and time and time again we’re being heard loud and clear.

Follow the Autoimmune Association on social media
Instagram: @autoimmune_diseases
Twitter: @AutoimmuneAssoc
Facebook: Autoimmune Association