It’s been 12 years since I apprehensively went to my GI’s office with my mom, trembling in fear about the what ifs and worrying about the pain of the injection and how my body would respond. One dozen years ago I threw caution to the wind and knew I needed to take the leap. I trusted my physician. There was no other choice. I knew I needed more to control my Crohn’s. I realized my quality of life depended on it. My present life and my future deserved more. 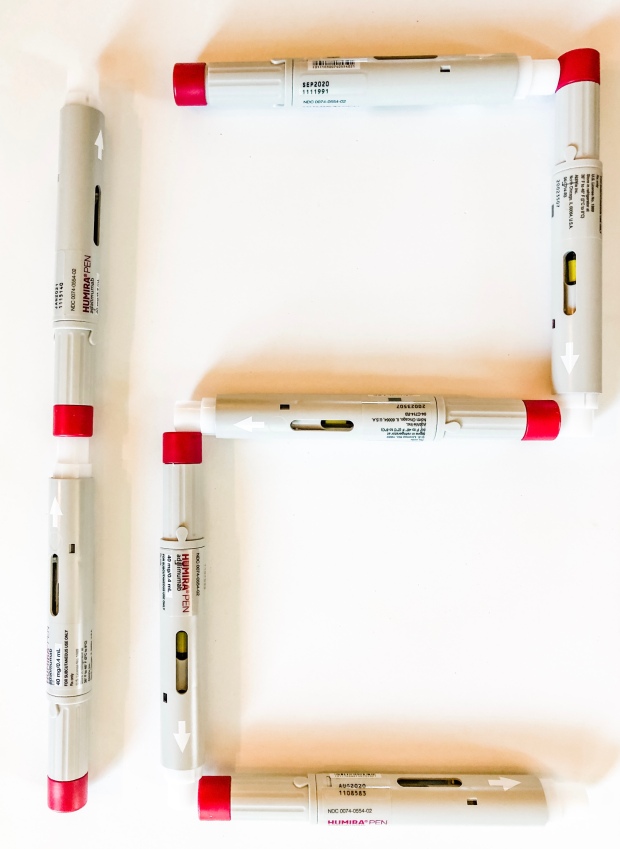
I wish I could tell that frightened 24-year-old girl that a biologic would enable her to fulfill her dream of working full-time in television, that she would go years between hospitalizations, that she would meet the love of her life, travel out of the country, and have two healthy children…all while on a biologic.
This week—I share my 12 tips for navigating life on a biologic and what I wish I knew 12 years ago today.
- Needing medication is not a failure. Not everyone has the luxury of being able to “heal their gut” solely with food and that is ok. You are not less than because you need to be on a biologic. You are not giving up or taking the easy way out.
- Side effects are unique to each person. Just because one person responded beautifully to a biologic, doesn’t mean that you will. The same goes with horrible side effects. One person’s experience has nothing to do with yours. IBD is unique in each one of us. While some people get a “Humira hangover” and are in pain leading up to their injection, others like me, deal with no side effects whatsoever. Don’t base your experience off anyone but your own and remember to consider the benefit vs. the risk.
- Google is not your friend. Prior to starting a biologic or when you are on one, it does you no good to Google and read all the doomsday laundry lists of “what ifs” and horror stories. If you want to educate yourself and truly learn more, communicate with your physicians and connect with fellow IBD patients who understand your reality.
- The drug fails you; you don’t fail the drug. Time and time again, I see patients say… “I failed Remicade. I failed Stelara. I failed Entyvio. I failed Humira.” You did not fail anything. This is not a blame game and how your body responds to biologics is completely out of your hands. If a drug doesn’t help limit inflammation and control disease progression, it fails you and you move on to the next.
- Have a routine and be compliant. Life gets hectic and being on a biologic must become a part of your routine. It’s helpful to keep track on a calendar or to set up an alert on your phone. I’m old school and write R or L in my day planner…meaning “Right Leg” or “Left Leg”…you’d be surprised, you won’t remember which leg you last injected two weeks ago. I’ve done my Humira injections on Mondays since 2008. I’ve always liked that day of the week because it doesn’t interfere with the weekend and I get it out of the way. No one likes Mondays anyways. Biologics aren’t just something you skip or can forget like a daily multivitamin. For the drug to work you must be compliant and stay on schedule.
- You can get pregnant and breastfeed while on a biologic. The most common question I receive from women with IBD is “can I get pregnant on my biologic?” and “can I breastfeed?” …the answer to both of those is a resounding YES. To safely bring a baby into this world, the mama’s health must come first. You need to be a safe haven for your baby and keep your IBD well-managed. By going off your medication, you put yourself at much greater risk for flaring while pregnant and after you deliver. I was on Humira until 39 weeks with my son and 37 weeks with my daughter. To learn more about biologics and family planning check out the IBD Parenthood Project and IBD Moms.

- Communicate openly with your GI. Check trough levels every now and then, especially when you’re feeling symptomatic to see if your drug level is therapeutic, if your dose needs to be increased, or if you’ve built up antibodies and need to possibly start a different biologic.
- Think about your lifestyle if you’re having trouble deciding which biologic to try. Back when I started Humira in 2008, there were only two biologics for IBD on the market: Remicade and Humira. At the time, I was a morning news anchor and did not share my Crohn’s disease with the public—so choosing to do an injection in the comfort of my home vs. being in public getting an infusion was a no-brainer. Now as a mom of two, I’m grateful for that choice. You can’t beat the convenience of being able to do a 10 second injection on your couch. I have so many friends who spend hours upon hours getting an infusion—having the stress of lining up childcare and allocating that much time and resources to get my medication would be a struggle for me. Let alone needing to get an IV…I know I’m not alone when it comes to having bad veins! I understand you need to go with what your body responds best to and what your physician recommends for treatment…but if the decision rests on your shoulders, I would absolutely choose injection over infusion.

Injections at home make chronic illness mom life a bit easier.
- Consider yourself “lucky” if you’re starting Humira now. The first 10+ years I was on Humira the injection was very painful. I know of people who had to take anti-anxiety meds just to feel comfortable receiving the injection. In 2018, the Citrate-free (pain free) version was released in the United States. Click here to watch my emotional experience doing an injection with the pain-free formula for the first time, while pregnant. This has been a game-changer for everyone on Humira, young and old. Self-injecting takes some getting used to, but it’s a hell of a lot easier now that you don’t have to deal with any pain. Chalk this up as a big win for the patient community—and if you haven’t made the switch to Citrate-free yet, make sure you do now!
- Drown out the Debbie Downers and the naysayers. You are going to come across friends and family who most likely have good intentions…but will question your decision to be on a biologic and offer useless, worrisome advice or stories of their friend’s friend who died from lymphoma or their boyfriend’s dad who had a bad reaction. I remember people questioning me about being on Humira when we were starting our family. We’re already worried enough, having to deal with the background noise can be the biggest pain of all.
- Be inspired by the possibilities. We’re all quick to expect the worse or struggle to imagine a life that doesn’t involve daily setbacks. Think of all the good that can come of this and the quality of life the medication can afford you with. Be patient with your body. Be patient with the drug. Be patient with yourself on this journey.
- Get preventative screenings. Stay on top of your appointments outside of your gastroenterologist. See your Ob-Gyn and get annual pap smears. See your dentist every six months. See a dermatologist and get an annual full body screening. Talk with your GI about getting “safety labs” every three months to keep a close eye on your results and make sure nothing is out of whack. See an eye doctor annually, even if you think you have perfect vision. Steroids can cause cataracts and IBD can cause inflammation around the eye. If your child has IBD, make sure to stay on top of pediatrician appointments. Being well-informed about all aspects of your health helps protect you from falling victim to any serious side effects.
BONUS: Reward yourself. Let’s face it. Giving yourself an injection or getting an infusion is not the most enjoyable experience. Think about how you can treat yourself when it’s over. Get some ice cream. Get a manicure. Order that cute pajama set online. Lord knows, you’ve earned it. If you struggle self-injecting, stare at a photo of a family member or friend that exudes strength and resilience, they will inspire you to be strong.
I’m not sure what the next 12 years will bring. Will Humira continue to be my go-to? Will there be a different treatment option? Only time will tell, but for now, I’m incredibly grateful that I’ve been able to stay on the same course of treatment for this long and I don’t plan on doing anything to rock the boat. My wish for you is that you’ll find a treatment that works its magic and shows you all that you’re capable of, despite your IBD.

In addition to the Humira, do you maintain a strict diet as well?
LikeLike
Hi! I don’t maintain a strict diet…I just stay away from my triggers (popcorn, nuts, too much caffeine/dairy, diet pop, limit alcohol, corn…other than that, I really eat everything and have been in remission nearly five years now. 🙂
LikeLiked by 1 person
Hi Natalie! Thank you for this great post! I needed to hear this. You said you were on humira for 12 yrs and you were only told you were in remission 5 years ago? What about the 7 yrs before while on humira did you still have flares?
LikeLike
Great question, Dinah! I wasn’t told by a GI until 2015 that I was in remission, but had many good years out of the hospital prior to that. I had a hospitalization in 2009…and then didn’t visit the hospital until fall 2012. From there I wasn’t hospitalized until winter 2014. Despite being on Humira, I still had three bowel obstructions along the way and had bowel resection surgery (all in 2014-2015). No biologic is a cure, but the medication has the ability to slow down disease progression and help people reach remission. Despite having the flares along the way, my physicians always kept me on the drug, as I haven’t built up antibodies and for the most part, have done really well on it. Following my surgery, which put me into surgical remission, I was told to stay on my biologic as my disease process is aggressive and staying off meds could have put me at greater risk for needing additional surgeries. Hope this helps! 🙂
LikeLike
This is a beautifully written piece. I started Humira for arthritis 17 years ago and it was life changing, as you say there is so much negative information avaliable it’s nice to hear a positive voice.
LikeLike
Hi Natalie, you mentioned you took humira until 38/39 weeks of pregnancy for both your kids. What did you take after that period and during breastfeeding? I have read that there is bigger risk of medicine passing placenta during 3rd trimester. I am 8 weeks pregnant and afraid to continue on this medication. Another question, when you are in remission does that mean you can stop this medication? Thanks!
LikeLike
Hi Veena, I took Humira until 39 wks with my son and 37 wks with my daughter (because my scheduled csection was the same day as an injection and the GI didn’t want the baby to get a burst of medication the day she was born in the month of January. (My kids are 3.5 and 21 months, both are perfectly healthy). I stayed on Humira throughout post partum and breastfeeding. Even when in remission, it’s important to stay vigilant in managing your disease and keeping it under control. As an IBD mom, I would not risk flaring by going off medication. This is an important conversation to have with your physician.
LikeLike